10 Common Symptoms of Diabetes
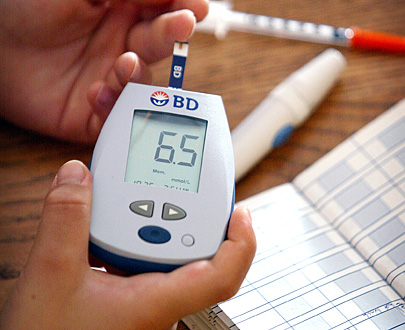
Diabetes has been coined the alarming name of the "silent killer" because the symptoms are easy to miss and many people aren't even aware that they may have diabetes. Over 24 million people in America have diabetes and more shockingly only about a 3rd of that number are aware that they have it. It's the disease where rising sugar can become a poison in your body. It is important to get a blood sugar test to determine whether you have diabetes. If you suffer from any of the symptoms listed here you should talk to your doctor immediately.
1. Increase Thirst & Urination
If you suddenly find that you need to go to the bathroom all the time and even have to get up in the middle of the night to go to the bathroom, you may have diabetes. It's because your kidneys are desperate to get rid of the extra glucose in your blood. You will become thirstier because your body then tries to replenish what is lost.
2. Weight Loss
Unless you are on a new weight plan you should be dropping weight for no reason. Weight loss is a common sign of diabetes because high sugar levels can cause rapid weight loss.
3. Fatigue
It's when the glucose in your body gets stored incorrectly, your cells then become energy starved which will result in you feeling less energetic and weak.
4. Hunger
When you have diabetes you will experience drastic high and lows in blood sugar levels which can make you feel hungry all the time.
5. Numbness
When your body experiences constant highs in glucose levels than damage can be done to your nervous system. Which in turn can cause a numb feeling in your body.
6. Skin Problems
Extreme dry skin and itchiness is a sign of diabetes. It happens due to poor circulation in the body.
7. Slow Healing
A common sign of diabetes is your body's inability to heal wounds effectively. You may find that a bruise or cut is healing a lot slower than normal. Blood vessels can be damaged extensively due to high glucose in your blood and it will hinder the healing process.
8. Yeast Infections
When you have diabetes it affects your immune system which makes you more susceptible to infections. The most common infection reported with diabetes is the yeast infection.
9. Irritability
Low blood sugar in anyone is bound to make them feel a little cranky. If your blood sugar has been low for awhile in can make you feel very unwell for a long period of time. When people feel terrible they find it hard to be in a good mood.
10. Problems with Vision
High blood sugar levels have been known to cause vision issues.
|
Is Swiss Chalet Festive
Special naughty or nice?
Megan Ogilvie
Toronto Star
DISH: The Festive Special
RESTAURANT: Swiss Chalet
LOCATION: Dozens of locations in the GTA
PRICE: $13.99
About the time Christmas carols start wafting through shopping malls, Swiss Chalet begins serving its Festive Special.
The quarter chicken dinner, served with a scoop of savoury stuffing, a dollop of cranberry sauce and a selection of chocolate truffles, is for manya long-standing tradition.
While we know the taste is holly jolly, few of us likely check whether the Festive Special is — nutrition-wise — naughty or nice.
The Dish decided to take on the task using the online nutrition calculator provided by Swiss Chalet. (Like Santa, we made a list, and checked it twice).
Unfortunately, that's not as easy as it sounds.
Despite the meal's popularity, Swiss Chalet does not provide nutrition information for its stuffing or cranberry sauce. Cara Operations Limited, the company that operates Swiss Chalet, did not provide a reason for this seasonal exception. After repeated requests, the company — through a public relations firm — did provide calorie content for the stuffing and cranberry sauce, but no other numbers.
The Festive Special in our photo is made up of a quarter chicken (white meat) with mashed potatoes and gravy, Chalet dipping sauce, a white roll with butter, stuffing, cranberry sauce and five Lindor chocolate truffles has 1,561 calories and at least 55 grams of fat and 2,310 mg of sodium.
For the average woman, that's 75 per cent of her day's calories, about 75 per cent of her daily fat allowance and just a tad more than the maximum recommended daily sodium allotment.
If you prefer dark meat and fries, the meal is definitely naughty. It has — and remember, this is without a drink or dessert — 1,846 calories. Registered dietitian Shannon Crocker says that is about what some women need for an entire day and about 75 per cent of the average man's recommended daily intake.
"In terms of calories, that is like eating six cheeseburgers from McDonalds. Or, seven Boston cream doughnuts from Tim Hortons."
The meal Crocker describes has at least 1,310 mg of sodium (remember, that's not including the sodium in the stuffing or cranberry sauce), or about 90 per cent of the sodium our bodies need in a day. And, Crocker says, the meal's 81 grams of fat (again, without the stuffing or cranberry sauce) is what you would find in 20 teaspoons of lard.
"This meal has double the fat some women should be eating in a whole day and about 100 per cent of that fat a man should get in a day," she says.
"With these numbers, you've basically got room for a light breakfast and only this version of the Festive Special — in one day."
The good news for festive special fanatics is there are ways to take the naughtiness out of the meal. Here are Crocker's tips to making the Festive Special nice:
• Order the quarter chicken with white meat and no skin to save a few calories and between 5 and 10 grams of fat.
• Skip the stuffing to save the 376 calories. It's also likely loaded with sodium.
• Ditch the fries to save 530 calories and 27 grams of fat. Even eating half will net substantial savings.
• The garden salad with fat-free raspberry vinaigrette is the most nutritious side.
• Swap the white roll for multi-grain to get a smidgen more nutrition out of the bread.
• Consider sending back the Chalet sauce. Yes, sacrilegious to some, but the little pot of sauce has 700 mg of sodium. If you love the Chalet sauce, be judicious.
• Eat just one truffle after your meal and save the rest for later. Consider them a mini advent calendar and eat one a day.
VERDICT: Depending on the choices you make, your Festive Special can be naughty or nice.
The Festive Special
A quarter chicken (white meat) with mashed potatoes and gravy, Chalet dipping sauce, a white roll and butter, stuffing, cranberry sauce and 5 Lindor chocolate truffles
Note that Swiss Chalet did not provide complete nutrition information for this meal. The below numbers do not include the fat, sodium, carbohydrate or protein content for the stuffing or cranberry sauce.
CALORIES 1,561
FAT 55 grams
SODIUM 2,310 mg
PROTEIN 61 grams
CARBOHYDRATES 86 grams
Quarter chicken, white meat with skin
CALORIES 290
FAT 11 grams
SODIUM 330 mg
PROTEIN 48 grams
CARBOHYDRATES 0 grams
Mashed potatoes with gravy
CALORIES 195
FAT 5.5 grams
SODIUM 1,010 mg
PROTEIN 4 grams
CARBOHYDRATES 34 grams
Chalet dipping sauce
CALORIES 25
FAT 0.5 grams
SODIUM 700 mg
PROTEIN 0 grams
CARBOHYDRATES 5 grams
White roll with butter
CALORIES 180
FAT 8 grams
SODIUM 245 mg
PROTEIN 4 grams
CARBOHYDRATES 22 grams
Stuffing
CALORIES 376
The Festive Special
A quarter chicken (white meat) with mashed potatoes and gravy, Chalet dipping sauce, a white roll and butter, stuffing, cranberry sauce and 5 Lindor chocolate truffles
Note that Swiss Chalet did not provide complete nutrition information for this meal. The below numbers do not include the fat, sodium, carbohydrate or protein content for the stuffing or cranberry sauce.
CALORIES 1,561
FAT 55 grams
SODIUM 2,310 mg
PROTEIN 61 grams
CARBOHYDRATES 86 grams
Quarter chicken, white meat with skin
CALORIES 290
FAT 11 grams
SODIUM 330 mg
PROTEIN 48 grams
CARBOHYDRATES 0 grams
Mashed potatoes with gravy
CALORIES 195
FAT 5.5 grams
SODIUM 1,010 mg
PROTEIN 4 grams
CARBOHYDRATES 34 grams
Chalet dipping sauce
CALORIES 25
FAT 0.5 grams
SODIUM 700 mg
PROTEIN 0 grams
CARBOHYDRATES 5 grams
White roll with butter
CALORIES 180
FAT 8 grams
SODIUM 245 mg
PROTEIN 4 grams
CARBOHYDRATES 22 grams
Stuffing
CALORIES 376
Cranberry sauce
CALORIES 120
5 Lindor chocolate truffles
CALORIES 375
FAT 30 grams
SODIUM 25 mg
PROTEIN 5 grams
CARBOHYDRATES 25 grams
RECOMMENDED DAILY ALLOWANCE
Men/Women
Calories: 2,500/2,000
Fat: 60 to 105 grams/45 to 75 grams
Sodium: 1,500 to 2,300 mg
Carbohydrates: 281-325 grams |
Canada approves first low-risk alcohol drinking guidelines
Ann Dowsett Johnston
Special to the Star
It's unanimous: Canada's first national low-risk alcohol drinking guidelines have been given the green light by Health Canada, as well as all provincial and territorial ministers at a meeting in Halifax. "Alcohol is a health hazard," says Deb Matthews, Ontario minister of health and long-term care. "It's really important that we now have national guidelines."
More than two years in the shaping, the guidelines — approved on Friday — had already received the blessing of the Canadian Public Health Association, the Canadian Medical Association, the liquor industry and more.
According to the new guidelines, women should consume no more than two drinks most days, up to 10 a week, and men should consume no more than three drinks most days, up to 15 a week.
All should plan for non-drinking days, ensuring that they aren't developing a habit.
Beyond the weekly limits, the guidelines also make reference to special occasion drinking: "Reduce your risk of injury by drinking no more than three drinks (for women) or four drinks (for men) on any single occasion."
"That we have all agreed on what the guidelines should look like — government, the alcohol industry and public health — is unique to Canada," says Michel Perron, CEO of the Canadian Centre on Substance Abuse (CCSA), which oversaw the shaping of the guidelines. "You will not find another country that has this level of congruence."
The guidelines are long overdue. Like most G8 countries, Canada has witnessed an uptick in risky drinking. Canadians consume 8.2 litres of pure alcohol on an annual basis — more than 50 per cent above the world average. "It's not that we drink," says Rob Strang, chief medical officer of Nova Scotia, "but how we drink."
And how we drink causes a lot of alcohol-related harm. "If a country has a $14-billion a year problem," says Perron, "and much of it stems from the use of a legal product, the first step is to explain how the product can be used, and how to decrease that avoidable cost. Much of that cost is preventable."
What is significant about the guidelines is that they were the first priority of the National Alcohol Strategy. This is an intelligent and comprehensive blueprint shaped in 2007 by an expert working group convened by the CCSA, Health Canada and what was then known as the Alberta Alcohol and Drug Abuse Commission.
This group, together with representatives from public health agencies, alcohol manufacturers, treatment agencies and alcohol control boards, produced "Reducing Alcohol-Related Harm in Canada: Towards a Culture of Moderation." This was a milestone effort, presenting 41 recommendations.
These new guidelines won't change the drinking culture overnight, but they will establish an important benchmark for Canadians. "Up until now, the fun factor has been different, depending on which province you lived in," says Perron, referring to the fact that Canada has had four different sets of guidelines.
What is most remarkable is that the guidelines have industry's approval. At several junctures, it looked like industry might walk from the table. "It nearly went off the rails many times," says one insider. They stayed.
"They certainly don't want to be caught out like the tobacco people were," says Peter Butt, who chaired the expert review committee.
Clinically, these guidelines are important for the medical community, key to screening and brief intervention — a tool known to be effective for helping problem drinkers.
The next step? Broad circulation and promotion of the new guidelines.
Ideally, the liquor monopolies will play a major role. "One of the advantages we have in Canada is the monopolies," says Perron. "Social responsibility is the primary justification through which the LCBO can maintain their monopolistic advantage. And social responsibility is not something you do — it's how you do things."
After that: standard drink labelling on all alcoholic beverages, articulating how many standard drinks are in each container. "Without them, it's like having a 100-kilometre speed limit and no speedometer on your car," says Perron. "How do you gauge consumption if you don't know how much you are drinking."
Strang agrees: "Industry loves to say they're all about responsible drinking, but how does their marketing and labelling portray responsibility?"
This could be a sticky point with the alcohol industry. Says Andrew Murie, CEO of MADD Canada: "I am not sure that the beverage industry is going to come singing 'Kumbaya' on this one. But like tobacco, it's a product where you need to warn the public."
These guidelines represent a healthy limit. But drinking to optimize health? That's another matter. "One drink a day—and that's a fairly unusual consumption pattern," says Tim Stockwell, executive director of the Centre for Addictions Research of B.C. Still, he points out, a daily drink is where "the risk of cancer starts."
If Stockwell had his way, Canada would move to warning labels: "If you can do this for tanning salons, why not alcohol? What other product do we protect when there is scientific evidence that use causes cancer? In this country, billions of dollars are made by governments on alcohol, and it causes the deaths of 10,000 or more each year. Consumers have a right to know. Of course, the alcohol producers might have trouble with this."
|
Use of stomach drugs
by seniors soars
Acid-reducing proton pump inhibitors are being prescribed to seniors 60 per cent more often than they were five years ago.
André Picard
Globe and Mail,
The number of seniors taking acid-reducing drugs to treat gastrointestinal woes has soared by 60 per cent over the past five years, newly released data show.
More than one in five Canadians over the age of 65 were treated with proton pump inhibitors (PPIs) in 2007-08, up from one in eight in 2001-02, according to the Canadian Institute for Health Information.
“Usage seems to be steadily increasing,” said Michael Gaucher, manager of pharmaceuticals at CIHI.
Part of the increase seems to be a switch from an earlier class of medication known as histamine-2 receptor antagonists (H2RAs), but there also seems to be an increase in acid-related conditions, he said.
PPIs and H2RAs are used to treat gastroesophageal reflux disease (GERD), reflux esophagitis and peptic ulcer disease. They are also used to eradicate Helicobacter pylori, a bacterium that causes ulcers, and to prevent and treat ulcers caused by routine use of medications such as painkillers.
There are many brand-name and generic PPIs.
The big sellers include pantoprazole (brand name Pantoloc), esomeprazole (Nexium) and lansoprazole (Prevacid).
Laura Targownik, an assistant professor of medicine at the University of Manitoba in Winnipeg, said the use of PPIs – which work by decreasing the amount of acid the stomach produces – has increased because they are effective and generally safe.
“We don't have a lot of other medications for these conditions,” she said.
In recent years, there have been a number of safety concerns raised in relation to PPIs. Their use, and long-term use in particular, has been associated with a higher risk of hip fractures, heart attacks and infections such as Clostridium difficile and pneumonia.
Dr. Targownik, who specializes in gastroenterology, said those risks must be kept in perspective and balanced against the benefits of the drug.
What is essential for patients and physicians alike, she said, is to ensure that use is appropriate, particularly long-term use.
Sometimes heartburn can be treated with over-the-counter acid neutralizers such as Tums, or with H2RAs such as Zantac. But in many instances, more powerful PPIs are the best choice.
“If there is a valid indication, then continue using PPIs. So I advise their use – with caution,” Dr. Targownik said.
Last year in Canada, there were 17.4 million prescriptions for proton pump inhibitors and sales totalled $1.3-billion, according to IMS Health Canada, a private company that tracks prescription drug sales.
About half those prescriptions were used by seniors.
CIHI's study was based on public drug insurance claims for Canadians aged 65 and older in six provinces – Alberta, Saskatchewan, Manitoba, New Brunswick, Nova Scotia and Prince Edward Island.
Over the study period, total drug program expenditures on PPIs across the six provinces increased at an average annual rate of 8.9 per cent – resulting in a doubling of costs to the public treasury over a five-year period. PPIs accounted for 7.3 per cent of total drug program expenditures last year.
|
Microchip spots cancer
quickly and painlessly
Megan Ogilvie
Joseph Hall
Toronto researchers have developed a portable device they say will accurately diagnose prostate cancer in 30 minutes.
The microchip technology, created by a pair of University of Toronto scientists, will be able to determine the severity of the tumours through a simple urine sample and produce quick diagnosis with no need for painful biopsies.
Now heading into the engineering stage, a BlackBerry-sized device should be available for doctors' use within two to three years and eventually could be tuned to detect a broad range of cancers and infectious ailments, the researchers say.
"The goal would be to produce a result ... while you're sitting in the waiting room," said engineering professor Ted Sargent, who holds the U of T's Canada Research Chair in Nanotechnology.
A paper on the work was published yesterday in the journal Nature Nanotechnology.
The device uses a fingertip-sized microchip – fitted with microscopic meshing – programmed to detect DNA sequences and proteins uniquely produced by specific cancers or pathogens.
These "biomarkers" would be drawn from urine or blood samples.
"We simply put a sample on the chip and we have a nice small chip reader that then analyses it and tells you what markers are in the sample," said Shana Kelley, a U of T pharmacology professor and study co-author.
Detected markers can tell you not only which kind of cancer is present, but also the stage and severity the tumour has attained.
"That's very important to be able to do that because cancers are actually a bunch of different diseases with different levels of aggressiveness," said Kelley. "Particularly in prostate cancer, there are very non-aggressive forms ... that you simply want to leave alone."
Kelley said the technology could herald an age of surgery-free diagnosis for cancer patients. "The real drive is toward non-invasive diagnostics so we can just screen people without having to take parts of their organs in order to do it," she said.
Dr. Tom Hudson, scientific director of the Ontario Institute for Cancer Research, said the study is "proof of principle" that it is possible to have a quick, affordable technology that can test for different cancer biomarkers at once.
"This is a critical step," he said. "They have shown you can detect this gene mutation (for prostate cancer). And if you extrapolate that you can do it for one gene, you could probably do it for 100 or 1,000."
Scientists are working hard to identify biomarkers for specific cancers and test those markers' usefulness in diagnosing cancer in patients. Some 1,000 biomarkers have been found, but Hudson said only nine of those have been validated so far in the clinic.
The other challenge is to find a way to test for many different biomarkers at once and develop a cost-effective technology to do it.
Hudson cautioned the device is still a long way off from being a staple in doctor's offices.
"How we make these (biomarker) tests happen in the clinic or in the clinical lab really needed some advances in technology. And Kelley and Sargent have done all the proof of principles here for a technology that's going to work."
For the initial work, Sargent and Kelley looked at prostate cancer, which has a set of signature biomarkers, shown in many studies to accurately portray the presence and severity of that disease.
The pair showed the chips were well able to pick up these makers in the minuscule concentrations typically found in the urine of prostate cancer patients.
But even now, Kelley said, they are shifting the technology's sights to other cancers and ailments.
"We've already done a little bit of work with head and neck cancer," Kelley said. "But really any cancer where there is an established molecular profile, we should be able to pick up using this device."
Sargent said he envisions the devices being a commonplace tool in doctors' offices around the world, along with a binder full of chips for different cancers and diseases.
"Say you were looking for H1N1 (influenza) or some dangerous infectious agent, there could be chips specific to those," he said. "You would just insert the proper one."
|
Great Lake fish alert:
Watch what you eat
Kenyon Wallace
Staff Reporter
As Ontarians flock to the Great Lakes for a little summer fishing, a new report is warning some categories of fish are unfit for consumption due to high levels of toxic chemicals found in their tissue.
"Fish are still great for our diets, but you need to watch what you eat," said Mike Layton of Environmental Defence, an author of the report.
"For the most part, eating a few small fish every month isn't a big deal but you should be cautious with larger fish that have had more time to accumulate higher concentrations of dangerous chemicals."
The report, entitled "Up to the Gills: 2009 Update on Pollution in Great Lakes Fish," brings together data from fish advisories published by the Ontario environment ministry between 2005 and 2009.
In many Great Lakes areas, high levels of mercury, PCBs, pesticides, dioxins and furanes were found in medium-sized and large fish (55 to 75 centimetres long) such as salmon, trout and carp.
Lake Huron catches showed some improvement but even there, cautions remained for larger fish.
Lake Ontario was less lucky, with 40 per cent of advisories saying eating certain fish in any quantity is unsafe. Many cautions targeted small and medium-sized fish, considered a disturbing trend.
"In the last two years, however, advisories for smaller fish in Lake Ontario levelled off," he said.
The "Up to the Gills" report can be seen at Environmental Defence's website.
|
Under pressure: How dangerous is Salt

Carly Weeks
Globe and Mail,
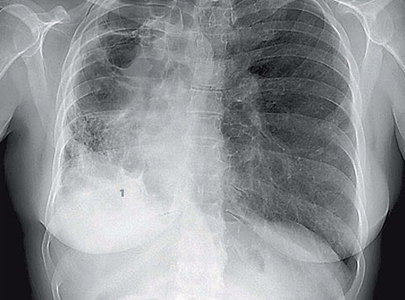
When David Beeching was taken to the hospital three years ago after breaking his leg skiing, he was anticipating X-rays, a cast and a painful recovery. He didn’t expect the news that he was suffering from a life-threatening condition.
Doctors told David’s family that he had seriously high blood pressure, a condition normally associated with the overweight and middle-aged. But David was neither of those things. He seemed fit and healthy – and he was only 13.
By the time he started receiving treatment, though, his heart was enlarged, indicating an elevated risk of cardiac attack or failure. Doctors prescribed medications, but most of all they ordered him to cut down drastically on salt – the prime suspect in causing hypertension.
David Beeching’s predicament is increasingly common among Canadian children and teens, and experts say it is due to the dangerously large amount of salt most of them consume – which for some can be sheer poison.
Hypertension may not sound so grim in itself, but it is a leading cause of heart disease and stroke, which kill more Canadians a year than anything but cancer.
Canadians overall take in about 3,100 milligrams of sodium a day – more than double the recommended intake for any age group and significantly higher than the upper limit most people can consume without compromising their health (2,300 mg, or roughly one teaspoon of table salt).
But a survey conducted by Statistics Canada in 2004 found that even toddlers were consuming more than 1,900 mg of sodium a day, nearly double what is recommended for them.
What’s more, 90 per cent of children 4 to 8 years old were not only consuming more than the upper tolerable amount of sodium for their age group every day – they were exceeding the maximum safe levels for adults. (For comprehensive figures, see sidebar, “A pinch to a binge.”)
High blood pressure and heart disease aren’t the only consequences. Excessive sodium has also been associated with an increased risk for stomach cancer, kidney disease, osteoporosis and asthma.
Doctors in Canada and the U.S., such as pediatric urologist Walid Farhat at Toronto’s Hospital for Sick Children, also have noted a rise in the number of young patients suffering from kidney stones – a disturbing trend they link to the way high sodium increases the body’s excretion of calcium.
“We see patients from the age of 1 all the way up to the age of 15,” Dr. Farhat says. “It’s all across North America.”
Reducing Canada’s salt intake is no simple matter, though. After David’s family got the news, says his mother France Savoie, she determinedly “scared him off” the habit of adding extra salt to his food. But since then, she has learned that putting away the salt shaker isn’t nearly enough.
Even though she’s a full-time nurse in Mont-Saint-Hilaire, Que., Ms. Savoie had never realized just how much of the sodium consumed by modern Canadians is already in the food we buy. Seventy to 80 per cent of it comes from packaged, processed foods in which sodium is relied on as a preservative and to enhance flavour.

That, of course, includes salty snacks such as potato chips and pizza. But some of the worst offenders are much less obvious, such as store-bought tomato sauce and breakfast cereal.
The Statistics Canada researchers didn’t even include salt added by the consumer. It was hardly necessary, given that a cup of Cheerios with a cup of skim milk, a cup of Campbell’s tomato soup and one large flax tortilla add up to more than the adult daily recommended intake – and that’s without having any dinner.
Now, Canada’s leading health experts are finally sounding the alarm that excess sodium is creating an entirely preventable public-health crisis. But so far Ottawa has done little to address the issue.
Five million Canadians have high blood pressure. Norm Campbell, a medical professor at the University of Calgary, says that simply reducing dietary sodium to nearer recommended amounts would eliminate one case in five.
“It’s almost negligent we haven’t done something about this before,” says Dr. Campbell, who was named the first Canadian Chair in Hypertension Prevention and Control by a group including the Canadian Institutes of Health Research in 2006.
Hypertension already costs the health-care system $430-million a year, and experts say that number will grow exponentially if something isn’t done about the extraordinary amounts of sodium consumed by children across Canada.
ROCK OF AGES
Salt has been a cornerstone of human civilization for thousands of years, helping empires expand, cities prosper and leaders crush their rivals. Before the dawn of refrigeration, salting was the best way to preserve meat, making it one of the world’s most valuable commodities.
Salt isn’t necessary to preserve meat these days. But the modern reality of two-income families and hectic schedules means that few parents now use fresh ingredients exclusively or make all meals from scratch. Packaged snacks, canned food and pre-made or frozen meals loaded with salt are now a normal part of family life. And so is the appetite for candy and junk food loaded with salt, sugar and fat.
Unknown to many Canadians, that has allowed sodium to creep into our diets at astonishing levels.
Research suggests that salt is addictive, making it very difficult to reduce consumption. It seems no coincidence, then, that many food companies use it as an inexpensive way to enhance flavour. Not all high-sodium products taste like it, usually because salt is masked by other ingredients such as sugar, herbs or spices.
Kids demand French fries, pizza, chips, hot dogs and candy, and their exhausted, time-pressed or indulgent parents hand it over. They may try to limit it, but the reality is that many kids eat too much junk. That fact is largely responsible for the childhood-obesity epidemic that has sparked widespread demand for junk-food advertising bans and physical-education reform.
Yet the average Canadian is less aware of the beating that high amounts of salt can inflict on the body, making it harder for the heart to pump blood and demanding extra work from the kidneys.
And it’s not just in junk food. Many foods promoted as healthy because they are low in fat, sugar and calories (such as canned vegetables and beans, lean cold cuts, whole-grain breads, fat-free salad dressings and ready-made soups) contain far more sodium than most people suspect.
Indeed, as the market for low-fat, calorie-wise and sugarless food products has exploded over the past few decades, the salt levels in many of these items have crept up, perhaps partly in compensation.
Studies have also found links between childhood obesity and high-sodium diets – children who eat more salt also drink more liquids, often turning to sugary pop and juice.
It’s not yet clear how rampant hypertension is becoming among children. Family physicians often don’t test for it, meaning that many children may have high blood pressure and not know it. In fact, it’s estimated that almost half of adults with the condition are unaware of it.
As health problems common to adults begin to emerge more frequently in children, the medical community has also grappled to understand what constitutes a dangerous blood-pressure reading in a child, whose body is much different from an adult’s.
Few people know why sodium should be a top priority on the public-health agenda better than Sheldon Tobe, a researcher in hypertension and kidney disease at Toronto’s Sunnybrook Health Sciences Centre who has spent the past few years as a spokesman on the subject for the Heart and Stroke Foundation of Canada. “Now is the time to really work on cutting back on salt in society,” he insists.
GETTING THE WORD OUT
But is anybody listening? For years, Canadians have heard that fat, sugar and high calories are the culprits in rising obesity and spikes in childhood diabetes. Unfortunately, the message was so well received that many parents consider only fat and sugar, not salt, before tossing a product in their shopping carts.
Now, as health advocates try to focus the same attention on sodium, parents are feeling unsure what is left to feed their kids that will not harm their health down the road.
It’s a problem Kim Horricks of Calgary lives with every day. Her 14-year-old daughter, Amanda, is seriously overweight, is at risk for developing diabetes and recently found out she is suffering from high blood pressure.

“She doesn’t tend to lean towards healthier foods, fruits and vegetables,” Ms. Horricks says. Amanda’s habits don’t include a lot of physical activity either. “She’s a teenager who loves her screen time.”
Ms. Horricks is trying to give more fruits and vegetables to her daughter as well her 12- and seven-year-old sons. But it’s far from easy. Her kids are picky eaters, and between work and errands, Ms. Horricks and her husband, Warren, seldom have the energy to cook from scratch. They tend to rely on packaged snacks for school lunches as well as oven-ready food that can be whipped into a quick dinner and the occasional pizza on the weekend.
When she reads nutrition labels, Ms. Horricks admits that she’s still in the habit of looking at fat, sugar and calories, not sodium – even though she has a child with high blood pressure.
Jennifer McIntosh, on the other hand, knows exactly how much sodium her 18-month-old son, Tyler, gets. Ms. McIntosh has a family history of high blood pressure and heart disease, so when her son was born, she became a dedicated label reader.
What she found startled her: Tomato juice, sauces and even baby food were “astronomically high” in sodium. She wondered, “How can they sell this?”
Instead of compromising on Tyler’s sodium consumption, Ms. McIntosh, who lives with her family just outside Montreal, made major adjustments to her shopping. She buys low-sodium products and has invested in a pressure cooker, which allows her to can her own stews and sauces.

She knows what a high-salt diet could do to her son’s health, and she is not about to let that happen.
Not everyone who eats a high-sodium diet will develop hypertension. Certain people – including those with family histories of hypertension, black people and those who suffer from kidney problems or diabetes – tend to be more sensitive to the effects of sodium and at greater risk for high blood pressure.
Some food companies and industry organizations such as the U.S.-based Salt Institute have used the sensitivity argument to criticize population-wide efforts to reduce sodium consumption, saying it’s unnecessary for most people. They have recruited doctors and scientists as experts to back their claims.
But even those who are not salt-sensitive today become more vulnerable as they reach their 40s and 50s. According to non-profit health organization Blood Pressure Canada, more than 90 per cent of Canadians who live to be about 80 will develop high blood pressure unless they take steps such as exercise and sodium control.
Catherine Yarema was only 28 when she found out during a routine physical that her blood pressure was high. Thinking that it may just have been nervousness, she continued to monitor it over the following months. Her readings kept worsening, and she decided to go to the hospital after experiencing intense headaches and heart palpitations.

A specialist prescribed two medications and told her that she would need to take them for the rest of her life. The doctor also instructed her to cut down on salt.
Two years later, last summer, Ms. Yarema found out that one of the medications had triggered an allergic reaction to gluten. She consulted with a dietitian and started to realize that even though she had long ago stopped adding salt to her food, her sodium intake was still high because of packaged, processed food.
“I was quite shocked,” she says. She had no idea that ditching the salt shaker wasn’t enough to control her intake.
Since then, Ms. Yarema, now 31, has completely changed her eating habits. In addition to avoiding gluten, she and her husband make all their soups, sauces and salad dressings from scratch, never adding salt. She brings a lunch to work religiously and no longer gives into the temptation of convenience foods.
Ms. Yarema saw her family doctor several times after she adopted her new diet. Each time, her doctor noticed an improvement in her blood pressure and lowered the dosage of her medication.
At a checkup in December, the doctor told Ms. Yarema that her blood pressure was completely normal and that she no longer needed medication – something she had been told could never happen.
AGAINST THE GRAIN
Catherine Yarema healed herself by changing her diet – now the nation of Britain is trying to do the same.
Five years ago, it became one of the few countries to act decisively on sodium by launching what is widely considered the world’s most aggressive reduction campaign. Many experts say it provides an excellent model for Canada.
Ottawa, however, appears to be in no hurry. The federal government created a working group to address the issue two years ago. Including representatives from federal agencies, the medical community, health-advocacy organizations and the food and restaurant industries, the group has met several times but has yet to develop a strategy.
“I think we would like to have seen greater progress,” says Kevin Willis, director of partnerships with the Canadian Stroke Network and member of the task force. Like hypertension researcher Dr. Campbell, Dr. Willis wants to develop strong measures to compel food producers to reduce sodium levels over time.
Food manufacturers and restaurants say they agree on targeting sodium but resist the idea of strict government regulation.
“I think there’s lots of evidence out there that a voluntary approach can work,” says Ron Reaman, vice-president of federal government affairs at the Canadian Restaurant and Foodservices Association, pointing to the measures taken in recent years to reduce trans fats. “I think that there’s incredible commitment on the part of the food industry to actually address sodium levels.”
With the consumer backlash over trans fats still fresh in the food industry’s memory, some companies already have moved to create low- or reduced-sodium alternatives. Nielsen market research reports that dozens of such products have begun to appear in the Canadian marketplace.
But many health experts say the current pace of sodium reduction is so sluggish that it’s putting lives at risk. They fear that leaving food companies and fast-food chains to their own devices won’t be enough.
“We’re taking in this substance, which is artificially added to our diet, at such high levels that it’s really acting as a chronic poison,” says Dr. Willis of the Canadian Stroke Network. “The only way in which we can really make an impact on sodium reduction in our diet is get manufacturers to reduce the amount.”
Meanwhile in Mont-Saint-Hilaire, three years after his diagnosis, David Beeching is about to graduate from high school. He dreams of becoming a musician, though for a living he expects to make and repair guitars.
As for his plans to manage his hypertension? “I don’t really think about it.”
But if he doesn’t start thinking about it, his mother worries that he could become a heart-disease statistic before he even turns 30. Despite her best efforts, Ms. Savoie can’t always force him to eat fresh fruits and vegetables. She knows the sodium in the bread, lasagna and French fries that David loves to eat outside the house is damaging his health. But she feels helpless.
“When you want to change yourself, it’s easy, but to try to change somebody’s habit, it’s not the same,” she says. “It’s really difficult.”
When salt has you licked
Reducing sodium consumption is not as simple as asking everyone to cut back. Not only do people love the taste of salt, but a significant amount of research suggests that sodium chloride (its chemical name) actually can be addictive.
According to David Kessler, former commissioner of the U.S. Food and Drug Administration, salty foods rewire the brain, making people prone to overindulgence and strong cravings. His new book, The End of Overeating, argues that consuming foods high in salt (as well as fat and sugar) change the way a person sees food.
A study published by the Elsevier journal Medical Hypotheses in 2006 found that a person who goes without salt experiences similar withdrawal symptoms as a drug addict. And the higher a person’s sodium consumption is, the greater will be his or her tolerance for more.
A person who switches from a high- to low-salt diet probably will consider the food bland and flavourless at first. But after a few weeks, the taste buds adjust, making the reduction less noticeable. A person who follows a low-sodium diet is likely to find the taste of high-sodium food excessively salty.
***
Salt in your system
Sodium
The body needs a certain amount of sodium every day to function; it is an electrolyte that helps regulate fluids and blood pressure and helps nerves transmit signals. Salt is also iodized in Canada to help prevent iodine deficiency, which can lead to mental impairment. (In many developing countries, this is a major cause of mental retardation.)
High blood pressure or hypertension
Blood exerts pressure on the walls of the arteries as the heart pumps it around the body. But if excess water in the blood vessels or increased rigidity in the artery walls force the organ to work harder, it can cause it to become enlarged, with the risk of heart attack, failure and other cardiac events.
Damage to blood vessels can cause them to burst or become blocked by a clot – if this occurs in the brain, it can cause a stroke.
Obesity, inactivity and excessive alcohol intake have been linked to high blood pressure, also known as hypertension. But high sodium intake has been shown to be the most significant factor.
Fatalities
In 2005, the latest year for which figures are available, heart disease and stroke accounted for 22.4 per cent and 6.1 per cent of deaths in this country respectively, according to Statistics Canada – more than any other cause of death except cancer.
The link
The correlation between increased sodium consumption and rising blood pressure is still not completely understood. It is known that excess sodium can cause the body to retain water. Extra water and sodium in the blood vessels means that the heart has to work harder to pump blood around the body.
Emerging research also suggests that a high-salt diet can stiffen the aorta and other central arteries, which could put increased pressure on blood flow.
Kidneys are vital to controlling blood-pressure levels because they remove extra sodium from the body and work to maintain a proper balance of sodium. Consuming excess sodium makes the kidneys work harder, and, in simple terms, can make them function less efficiently.
A safe solution
Most medical experts agree that government- and industry-led efforts to reduce sodium in packaged and processed foods won’t cause Canadians to become sodium- or iodine-deficient, because the mineral is ubiquitous in the food supply.
***
Our sodium levels
The average Canadian consumes twice the recommended amount of sodium per day – men more than women, with teenaged boys by far the worst offenders.
Recommended daily intake (amount of sodium adequate to good health), by age group:
- Ages 1-3: 1,000 milligrams (less than half a teaspoon of salt)
- Ages 4-8: 1,200 mg
- Ages 9-50: 1,500 mg
- Ages 51-70: 1,300 mg
- Over age 70: 1,200 mg
Daily tolerable-consumption limit (highest amount of sodium before significant risk of compromising health), by age group:
- Ages 1-3: 1,500 mg
- Ages 4-8: 1,900 mg
- Ages 9-13: 2,200 mg
- Ages 14 and older: 2,300 mg (roughly one teaspoon)
Actual average daily sodium intake in Canada, excluding salt added while cooking or at table:
Actual average daily sodium intake in Canada by age group and gender, excluding added salt:
- Ages 1-3: males, 1,918 mg; females, 1,918 mg
- Ages 4-8: males, 2,677 mg; females, 2,677 mg
- Ages 9-13: males, 3,513 mg; females, 2,959 mg
- Ages 14-18: males, 4,130 mg; females, 2,938 mg
- Ages 19-30: males, 4,066 mg; females, 2,793 mg
- Ages 31-50: males, 3,607 mg; females, 2,806 mg
- Ages 51-70: males, 3,334 mg; females, 2,573 mg
- Seniors over age 70: males, 2,882 mg; females, 2,300 mg
Source: Statistics Canada’s Canadian Community Health Survey
Carly Weeks is a reporter for Globe Life.
|
Prostate test may
not save lives

Megan Ogilvie
and Joseph Hall
A pair of huge studies published yesterday cast doubt on whether a popular prostate cancer test saves lives, but the head of the country's largest prostate cancer support group insists it saved him – and hundreds of other members.
Aaron Bacher of the Toronto Man to Man Prostate Cancer Support Group said he will continue to promote the simple PSA blood test as the best way to catch the cancer at its most treatable stage.
"I have no doubt the PSA test saved my life," he said. "I survived because the cancer was caught early and treated."
Two trials, published online yesterday in the New England Journal of Medicine, show the prostate-specific antigen test does little to reduce a man's risk of dying from the disease. They also suggest large-scale PSA testing may lead to more suffering than would the disease it aims to detect.
Dr. Anthony Miller, a study co-author and associate director for research at the University of Toronto's Dalla Lana School of Public Health, said the studies show the test should be used with caution.
They provide "very strong evidence" that a high proportion of cancers detected by PSA testing never would have harmed the men during their lifetimes, Miller said.
"So the detection of prostate cancer was unnecessary and potentially hazardous, and the complications (from surgery) that many of them have suffered – impotence, incontinence – were all unnecessary," he said.
The test, although at risk of yielding false positives, is not itself harmful, but it can trigger a cascade of debilitating treatments – including invasive surgery, radiation and chemotherapy – in cases where the cancer detected would not be lethal.
Cancer experts have eagerly awaited the results of the two trials, which collectively involved more than 230,000 men in the United States and seven European countries. Up until now, there had been no conclusive evidence whether the PSA did more good than harm.
The studies do not close the debate on the PSA test's long-term benefits, but experts say it provides valuable information on the test's potential risks and benefits.
In January, Ontario expanded its funding for PSA testing to include those ordered by a family physician. Previously the test, which costs between $30 and $50, was covered only when ordered at a hospital and paid for by that hospital's operating budget.
Dr. George Pasut, vice-president of prevention and screening for Cancer Care Ontario, said the two studies reaffirm most Canadian guidelines on PSA testing, which already caution health-care providers not to over-prescribe the test and recommends a well-informed discussion with patients to outline benefits and consequences.
"That is what most guidelines recommend ... And I would say both trials, in their separate ways, really reaffirm that," Pasut said.
Prostate cancer is the most common cancer among Canadian men. Last year, an estimated 24,700 males were diagnosed with the disease and 4,300 died from it.
Cancer experts had long hoped the test, which looks for elevated levels of PSA, a protein produced by the prostate that rises in the presence of cancer, would help prevent men from dying of the disease. The two trials cast doubt on that.
The U.S. survey looked at nearly 77,000 men, about half of whom underwent aggressive PSA screening involving six blood tests a year and four rectal exams. The other half was assigned to the regular care of their own doctors, of which half reported having at least one PSA test by the trial's seventh year.
The study, which is ongoing, found about 20 per cent more cancers were detected among men in the aggressively screened group than in the control group. But having the test did not reduce a man's risk of dying from the disease in the first seven years of follow-up.
The seven-country European trial looked at 162,000 men aged 55-69. That trial found no benefit of screening in the first seven years of follow-up care, but did hint PSA screening may prove slightly beneficial with the passage of more time. At nine years of follow-up, there were 20 per cent fewer deaths from the cancer in the screened group.
Dr. Christine Berg, the report's senior author and head of the U.S. National Cancer Institute group running the U.S. study, said PSA testing is almost certainly causing unnecessary suffering in men who receive treatment for cancers they would very likely never die from."Clearly we want to prevent deaths from advanced prostate cancer," Berg said. "But at the same time we want to minimize men living for 15 or 20 years with incontinence from a (prostate removal) that they didn't need."
Berg said positive PSA tests often provoke overly aggressive responses by physicians. "We need a less knee-jerk response to one isolated PSA level," she said.
Toronto Star |
14 questions about your heart
Our health reporter talks to a cardiologist about your heart, it's job and how to treat it right on Valentine's Day February 14, 2009

Megan Ogilvie
HEALTH REPORTER
Today is the day when hearts abound, from the creamy chocolate variety to puffed-up balloon heart bouquets to hearts snipped from pink paper, signed with love and sealed with a kiss.
So perhaps today, in the midst of these confectionary hearts, is the best time of the year to pay tribute to your physical heart – that most important organ that thump-thumps, thump-thumps inside your chest.
To get you started, we asked Dr. Paul Oh, medical director of the cardiac rehabilitation and secondary prevention program at Toronto Rehabilitation Hospital, 14 questions about the heart – about its job, its role in love and how to treat it right on Valentine's Day.
What fascinates you most about the heart?
The heart beats 100,000 times a day, about 37 million times a year and about 26 billion times in your lifetime. It's amazing that it can get through that lifespan, for the most part, in a pretty healthy state.
An analogy that I like to think about the heart is: The heart is like a home. It has got walls. It has got rooms and doors. It has got a plumbing system. An electrical system. And all of these need to keep running for 70 or 80 or 100 years. So there are opportunities for things to go wrong unless we maintain it right. And therein lies our challenge: When we're not maintaining, problems will arise in our plumbing or electrical system, or in the structure of the heart.
Is it, do you think, an under-appreciated bit of our body?
Yes, I think the heart is taken for granted, for the most part. We don't have to think about it; it just does its duty so effectively every single day.
The fact that most people don't eat properly, don't get enough exercise, means that we're not maintaining our home particularly well. We're creating the environment where things can break down.
Is there a time in our day or a time in our lives when we should appreciate the heart the most?
First thing in the morning is always a good time to appreciate your heart because it has started and (Oh chuckles as he says this) the alternate is never very good.
There are key moments in our life – the milestones of birth, death, marriage, children. These important life moments should be celebrated and maybe it is a good time to pause and be grateful for our health and our heart health in particular.
You work to help people rehabilitate their heart. What does that mean to you?
We work mainly with people who have suffered a major heart event – that is, they've had heart attack, angioplasty or major surgery on the heart. So they've taken a major knock to their health. We help them get back on their feet through exercise, lifestyle, and psychological and physical retraining to regain their health and, hopefully, help them feel better than they have in a long time.
Do you find that people have a better appreciation of their hearts after having a health problem?
I would say a definite yes. That if you faced a potentially life-threatening crisis or you become aware of problems that you're developing with your heart, I think it makes you appreciate your health even more. Hopefully, it creates a sense of greater motivation to do something about it.
Do some people have bigger hearts than others?
Yes, people do differ in their heart size. Heart size to some degree is related to body size. So bigger individuals will have slightly bigger hearts. Those who use their hearts more, athletes in particular, develop positive enlargements of their heart. They can thicken their muscles just like you might grow your bicep bigger, and also stretch it so it can accommodate a larger blood volume to pump things around.
How can you tell if your heart is healthy – without going to the doctor for tests?
The main way is listening to how your body is functioning. If you're able to get out and do a reasonable day full of activities – walking to and from shopping or work or playing with the kids – and you're feeling good with that – there is no chest discomfort or shortness of breath, arm discomfort, feelings of nausea or heartburn – then, by and large, you're doing pretty well. The body is pretty good at telling us when it's starting to get into trouble.
What is the biggest myth or misconception people have about their hearts?
The myth that is popularized is that heart disease is only a man's disease. And we know that this is completely false. Heart disease is the Number 1 killer for women, as it is for men. Not that cancer is not important but, for instance, heart disease is seven times more common than breast cancer for women. So it's an important health issue.
Women are different because sometimes recognizing heart disease is more challenging – they may not have the typical features of central squeezing chest pain, they may have more subtle symptoms of fatigue, shortness of breath or disturbances in sleep, which may be the clues that something is going on with heart disease. When a woman has risk factors, such as high blood pressure or diabetes or cholesterol abnormalities, these things can carry a much greater weight than it can for men. So it's important that women really recognize what is going on and advocate for attention.
Now, how about old wives tales? This may be out of your area of expertise but is there any truth to the old saying, `Cold hands, warm heart?'
I don't know if there is a really good correlation here. If you're exposed to cold and your hands get cold, you can certainly have a warm, loving heart still. Of the patients that I see, I actually get a little concerned when they have cold hands, because that could be a sign their circulation isn't very good and their hearts, while being warm, may be weak. That may be a bit of a concern for me.
Are there any other ones that you've heard in your career?
Um, no. I get questions but very specific questions about the heart, medications, blood vessels. So it's more physiological stuff.
It's Valentine's Day, and everywhere hearts are being pasted to walls, cards and cookies. Again, this is perhaps out of your realm but do you know why – or do you have any thoughts on why – the heart is a universal sign of love?
I think we can go back to the early scientists who thought the heart was the seat of the soul, the seat of emotion. As the source of blood flow for the entire body, the thought that spirit and emotion might be centred there is not far-fetched. So that if you had a healthy heart, then good things will flow from there.
I think also that people recognized early on that when we're emotionally driven, perhaps in love, that our hearts will beat faster, we may become flushed as our blood vessels are reacting, we may get the sense of fluttering in the heart as our hearts beat faster.
Does being in love (or out of love, for that matter) have an effect on your heart?
I think it probably could. We know that depression is very closely related to heart health, probably through a few mechanisms. One is that mental happiness or mental anguish has physiologic effects on the body by causing changes in stress hormones, such as cortisol, and that can have a direct effect on blood pressure and your heart.
We know that people who are not attached in relationships, who may have depression or social isolation, have a higher prevalence rate of heart attacks, for instance.
What's the best thing someone can do to care for their Valentine's heart today?
Make a conscious effort to improve your heart health with your Valentine. Have a lovely, healthy meal, take a walk and revel in the emotional and psychological support you provide for each other. These are the keys to heart health.
As we were chatting, a press release from participACTION came into my email box urging couples to "get it on" as a way to get more exercise on Valentine's Day. Any thoughts?
Certainly, sex can count and sex is a very important part of a healthy relationship. Sex can be viewed as a physical activity, which is both a positive and a caution. For those who are healthy, engaging in regular relations can be viewed as one of your more fun kinds of workouts, with all of the added bonuses of the emotional components that come with it.
For those who might be living with heart conditions or at risk of heart conditions, sexual relations may be viewed as a rigorous kind of activity so you need to be prepared for it.
How do you know if you're physically ready? Our rule of thumb here at the cardiac program is if you can walk up a couple flights of stairs without getting short of breath, you're probably ready for relations.
|
Salmonella recall list grows
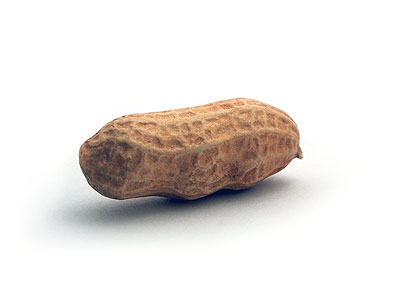
THE CANADIAN PRESS
The list of peanut products recalled in Canada over salmonella concerns continues to grow.
The Canadian Food Inspection Agency has added another 30 different products that are manufactured in Canada, and another American made product.
Most of the new products added to the list are various types of peanut, caramel and protein bars, and ice cream cones.
The federal agency says no illnesses are reported as a result of consuming the products now added to the list.
It comes as food tracing efforts uncover more products made with peanut butter from a Georgia supplier at the heart of a massive salmonella outbreak in the United States.
On Friday, the U.S. Food and Drug Administration also announced a U.S. and Canadian recall of peanut butter cookies and cookie bars made by Arico Natural Foods Company of Beaverton, Ore. CFIA has not announced that recall as of Friday afternoon.
thestar.com |
Health plan
funds killer drug

Publicly paid prescriptions for potent, often-abused painkiller skyrocket – and so does the death rate
Kevin Donovan
STAFF REPORTER
Public dollars are funding a dramatic rise in the use of narcotic pain pills that are killing more and more people in Ontario every year, a Star investigation shows.
Last year, doctors prescribed $54 million of OxyContin – called "hillbilly heroin" by street dealers – under a provincial program that provides free medications to people on social assistance, seniors and people with disabilities. That's nearly triple the $19 million handed out five years before.
Meanwhile, addiction rates are soaring and an estimated 464 deaths in five years in Ontario have been blamed on the drug contained in the pain pills, with the number steadily increasing each year.
"It's an epidemic," said Dr. Graeme Cunningham, a leading expert in addiction treatment. "We are seeing broken families, violence, police involvement."
Cunningham and others who have studied the impact of the drug believe there are two contributing factors.
Some doctors are too quick to prescribe OxyContin, the brand name of the drug oxycodone, giving it to people who do not really need it.
Also, some patients lie to doctors about symptoms to obtain the drug for trafficking.
Properly used, the drug's manufacturer, Purdue Pharma, says it can benefit people with chronic pain.
But addiction experts say the potent pills are too often trafficked to users who crush the slow-release tablets and snort or inject the drug. A pill that costs the public plan $4 at the pharmacy fetches up to $45 on the street and gives users an instant high.
It is as addictive as heroin and critics say users are not properly warned of its dangers.
Purdue Pharma and three top executives were fined $635 million in the U.S. two years ago for failing to properly warn consumers. The executives were put on five years' probation after a plea agreement ended the criminal prosecution.
OxyContin is rapidly becoming one of the top medications prescribed by doctors under the Ontario Drug Benefit program (ODB). The public assistance plan covers a quarter of the people in Ontario, but funds half the OxyContin prescriptions in the province. Private drug plans have also seen a growth, but at a slower rate.
Ontario is now grappling with a problem that first surfaced in the U.S. in the mid-1990s, and has dogged Atlantic Canada since the early 2000s.
A rise in OxyContin use in the U.S. led to crime waves and death, particularly in rural areas.
In Ontario, no one is willing to put a figure on it, but most agree some of the province's publicly funded narcotic is being misused.
Ontario's Centre for Forensic Sciences told the Star the estimated number of deaths attributed to oxycodone – OxyContin is a slow-release brand of the drug – reached 123 in 2008, up from 63 in 2004. In total, there were 464 deaths over the past five years.
The provincial health ministry committee that oversees the Ontario Drug Benefit program calls the dramatic increase in OxyContin use a "public health concern."
Last month, the Centre for Addiction and Mental Health (CAMH) released a study showing the greatest increase in patients seeking treatment for narcotic addiction from 2000 to 2004 came from people hooked on OxyContin.
A study by another agency showed increased use of OxyContin among teenagers in Ontario. It's become a party drug, with teens taking it at the same time as they drink alcohol.
Even the drug's manufacturer is worried. "There's a lot of prescription fraud and pharmacy theft," said Purdue spokesperson Randy Steffan. "It is certainly a growing issue."
The Star's investigation began with a detailed look at provincial data showing prescriptions paid for by the government and dispensed at retail pharmacies.
About half the OxyContin Purdue Pharma sells in Ontario is paid for by the public ODB plan. In 2007-08, the total ODB bill for OxyContin was $54 million, representing 337,000 separate prescriptions. Two-thirds of the people receiving the drug are on social assistance.
The per-pill cost at the pharmacy depends on the strength: the 10 mg dose is 92 cents under the ODB; the 40 mg pill is $2.39; and the 80 mg. pill is $4.41. The more potent the pill, the higher its street value.
The amount of OxyContin prescribed under the ODB has grown steadily for five years, with annual increases of roughly $8 million.
Ministry of Health spokesperson Andrew Morrison said the government believes drugs like OxyContin are "an important therapeutic option for the management of cancer and non-cancer-related pain."
He said the ministry is aware of the risk of abuse, and said that is why the drug is listed as a "limited-use product" on the ODB program, meaning it is only to be prescribed to patients with chronic pain.
OxyContin is the brand name of an opioid pain pill composed of oxycodone, first developed in the early 1900s. Oxycodone became popular as a one-shot painkiller in drugs such as Percocet, which are also often abused.
In 1995, Purdue Pharma obtained U.S. approval for a slow-release form of oxycodone that would provide pain relief for 12 hours. Within a year, communities were struggling with addiction problems as people learned to crush and snort or inject the drug for a rapid dose.
West Virginia, Tennessee and Kentucky were first and hardest hit. The nickname "hillbilly heroin" came from there.
Purdue's Steffan said his company does its best to inform the public of the risk of addiction by educating doctors. Purdue is aware of the rising death rate and "it reminds us that prescription drug abuse is a serious public health problem."
Steffan encouraged the Star to speak to pain medicine experts, including Dr. Roman Jovey, a family physician paid by Purdue to conduct workshops, lecture, and train doctors.
"(OxyContin) is an effective drug when given to the right person for the right reason," said Jovey, medical director of a chain of clinics called the Centres for Pain Management and also the director of Credit Valley Hospital's addiction program in Mississauga.
Jovey said one in five Canadians suffers from pain daily; he prescribes "lots" of OxyContin and thinks more people should be taking the drug or other pain medication. However, he said the government should also fund other types of pain treatment, such as physiotherapy and psychological counselling.
In their absence, Jovey said doctors and patients have little choice but to turn to OxyContin, which is covered by the public program.
"Unfortunately, a huge market has developed on the street, particularly with people aged 16 to 25," he said.
Meanwhile, addiction experts are sounding the alarm. A study of CAMH's Toronto in-patient service saw the number of people suffering from OxyContin addiction go from 3 in 2000 to 92 in 2004. (Updated figures were not available.) In a recent five-year period, there were 39 heroin deaths in Ontario, compared to 464 oxycodone deaths.
Cunningham said pain has become fashionable and profitable to treat. He and Jovey sometimes spar at debates over the issue.
"OxyContin is way over-prescribed, in my opinion," said Cunningham, director of the centre's addiction division. Of 1,500 new patients the centre sees each year, 600 are drug addicted. Nearly two-thirds of them are hooked on OxyContin and other, less potent prescription narcotics.
Last week, a new patient at his clinic had to "snort 120 mg of OxyContin just to get the courage to come in to get help for her addiction." Cunningham said the drug has a "tremendous euphoric effect" on people.
In Toronto, Daniel Roppa, 22, got off Oxycontin two weeks ago. He paid up to $1,000 a week to buy the drug illegally for the past year.
He got the pills first from friends, then dealers, who charged him $30-45 for each 80 mg. tablet. He does not know where the dealers got their supply. "All I cared about, after a while, was hanging onto a dealer. That was like gold."
On his worst day, Roppa recalls taking four pills twice a day, crushing and snorting them.
"I got so I was spending so much money on this stuff just to survive. Two weeks ago I broke the cycle, tested negative on my urine test and I am like a new man," he said.
"I call this drug the devil."
Data analysis by the Star's Andrew Bailey
Toronto Star |
Vitamin D boosts mental
health in elderly
Vitamin D can help fight off mental decline in the elderly, the BBC reports. In a study of 2,000 people aged 65 and over, researchers from the U.S. and the UK found those with lowest levels of vitamin D were more than twice as likely to have impaired mental ability.
The vitamin, which boosts bone health, helps with the absorption of calcium and phosphorus, and protects the immune system, is produced by sun exposure. Yet, as people age, their skin has a harder time absorbing it from the sun—a real problem in countries with long, dark winters like Canada. Seniors, then, must obtain vitamin D from other sources, like oily fish or fortified food products (including milk and cereal). Based on this research, providing the elderly with supplements might be beneficial, one researcher suggests: “We need to investigate whether vitamin D supplementation is a cost-effective and low-risk way of reducing older people’s risks of developing cognitive impairment and dementia,” says one British doctor.
|
Distracted easily? You're getting older
Megan Ogilvie
HEALTH REPORTER
Reading the newspaper? Studying for a test? Trying to balance the bank book? It might be best to turn off the TV.
Toronto scientists have found further evidence that older adults have a hard time tuning out distractions when concentrating on a single task.
The new research, reported yesterday, suggests older brains are less able to filter irrelevant information from the environment than the brains of younger adults.
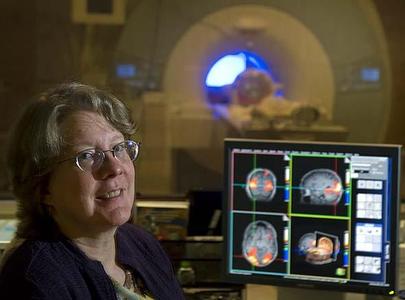
This seems to make it more difficult for older adults to focus on the task at hand, said study lead author Dale Stevens, who conducted the research at the Rotman Research Institute at Baycrest as a doctoral student at University of Toronto.
It is known from behavioural studies that older adults are more easily distracted, but this is the first to look at what is going on in the brain when people try to form a memory and fail, said Stevens.
"This certainly is consistent with the way we understand the problems older people might encounter when encoding information in everyday life," said Michael Rugg, director of the Center for the Neurobiology of Learning and Memory at the University of California, Irvine.
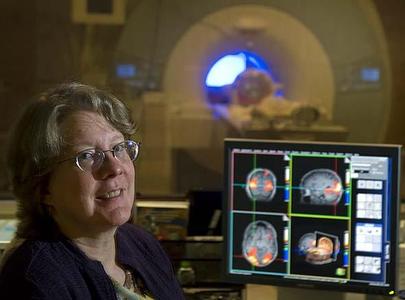
Stevens and his colleagues used functional magnetic resonance imaging (fMRI) to scan the brains of 12 younger adults and 12 older adults.
The groups were shown pictures of faces and were later asked whether they recognized any.
When both groups failed to recognize a face, the researchers saw decreased activity in the memory encoding regions of the brain, including the hippocampus, something the researchers expected.
But when older adults looked at faces they later forgot, their brains showed increased activity in a region that should have been quiet during memory encoding – the auditory cortex, the part of the brain that processes sound in the environment. The group of older adults had an average age of 70.
"This indicates that older adults were not able to suppress or filter out the noise of the fMRI machine," said Stevens. "We did not see this in the younger adults at all."
As it scans, an fMRI machine makes loud, repeated knocking noises.
Rugg said the study, published yesterday in the Journal of Neuroscience, suggests auditory distractions may prevent older people from properly filing memories.
Toronto Star |
Walk faster - you'll
live longer

Gait speed could help predict how long you'll live. It may very well be another important vital sign, like heart rate, blood pressure and cholesterol levels.
The magic number for staying young is 3.6 kilometres an hour. Why? If you can walk that fast, you are better able to bounce back from an illness. That's why zippy over-65 walkers in a recent study enjoyed lower mortality rates.
So, time yourself (or your mom or dad) on a tread- mill or around the track. Get your speed up by intermittently picking up the pace for a short distance on a walk or a treadmill.
One easy way to increase your pace is to do it by the clock: For the first 10 seconds of every other minute, walk faster. Each week, keep up the faster pace longer.
Once you've got your walking mojo going, add some strength training, which will help you get faster as well as stronger. And walk every day.
Anger is a pain in the lungs
That fight you had with your spouse or the feelings you have for that son-of-a-rhymes-with-witch who cut you off on the highway may keep you from breathing easy. And that prevents your body from getting what it needs to operate your other systems.
Yes, you pay twice with anger: It hurts your lungs.
Although lung function naturally declines as you age, it may slip faster in perpetual hotheads. In one study, men who scored highest in hostility performed poorly on lung function tests, both at the beginning of the study and years later. Strong negative emotions seem to provoke inflammation and alter hormone function, which can knock the wind out of your lungs' sails.
Also, the kind of bad feeling that piggybacks on anger often goes hand-in-hand with smoking and inactivity. Each of these – anger, unnatural hormone levels, smoking and inactivity – goads the others to make lung function worse.
Next time you're seething (but not while driving), try this: Close your eyes, relax and imagine yourself far away from what's making you so mad. Breathe deeply with your forefinger on your navel and feel it move in and out.
Then see what kind of results you can get without yelling.
GOT A COLD? GET OVER IT
Three things help reduce the average time a cold lasts, from roughly five days to three. Do any of these the minute you start feeling cold symptoms:
1. Chicken soup: Have one cup four times a day. Ingredients in grandma's favourite remedy have anti-inflammatory properties that prevent certain white blood cells (neutrophils) from migrating to your airways and contributing to the inflammation that causes annoying cold symptoms. Chicken soup also contains compounds that help inhibit mucus production, and its heat and steam may help open nasal passages.
2. Vitamin C: Wash down 500 milligrams of the vitamin with plenty of water four times each day. It's not clear why this works, but research has shown that it does.
3. Zinc lozenges: Take one every six hours. Your immune system needs zinc to function. Just don't try taking zinc lozenges every day as a preventive step. Taking more than 100 mg of zinc daily over a long time actually hurts, not helps, your immune system. (Lozenges generally have around 13 to 20 mg of zinc.)
MORE with LESS MEAT
A little less meat (beef, pork, veal, lamb, elk, luncheon meats, sausage, etc.) on your plate could mean much less meat on your bones. People who eat few or no animal products are less likely to be overweight or obese than people who eat meat.
Not enough to scare you out of the steakhouse? Consider this: Dropping meat lowers your risk of diabetes and heart disease – in fact, postmenopausal women who substituted vegetable protein for their usual red meat lowered their coronary heart disease death rates by a whopping 30 per cent.
You don't have to go cold, uh, tofu. Just choose appropriate portion sizes and low-fat cooking methods. A serving of meat is equal to 85 grams (3 ounces), about the size of a deck of playing cards. Limit red meat to one serving per week, and don't overcook it.
When you trim the meat, fill the nutrition hole with enough protein, vitamins B-12 and D, calcium, iron and zinc. Get them with soy products such as tofu or soy burgers; legumes, lentils or garbanzo beans; low-fat dairy; dark green, leafy vegetables; nuts; and whole grains. And add a vitamin supplement twice a day as an insurance policy against an imperfect diet (do that even if you have meat).
A LITTLE BEND, A LOT OF BENEFIT
These days, yoga gets more love than the current So You Think You Can Dance star. And for good reason: It increases three "relax-it's-okay" compounds in your body. Best of all, you can get its rewards even if you're about as pliable as a two-by-four. Talk about a natural high.
Yoga boosts blood levels of serotonin, dopamine and endorphins – three natural feel-good substances. This ancient practice may boost mood even higher by preventing middle-age weight gain. One study found that it helped adults between the ages of 45 and 55 maintain or lose weight when they practised regularly for four years or more, as opposed to the pound-a-year gain that happens to most people.
And the effect of yoga on overweight people was especially dramatic: They gained 18.5 pounds fewer than those who did not practise.
So downward-dog it: You've got nothing to lose ... except maybe some mental and physical weight.
The You Docs, Mike Roizen and Mehmet Oz, are authors of the best-selling YOU: On a Diet. Send questions to the good doctors on their website, realage.com.
|
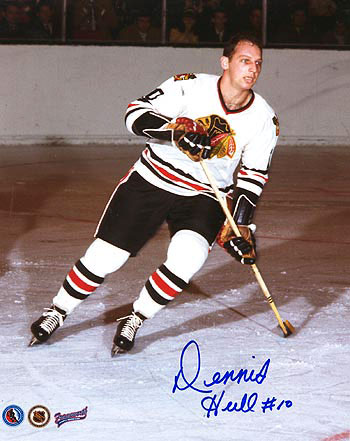
DENNIS HULL Spotlight on COPD
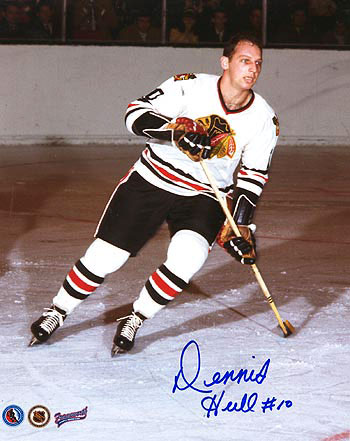
On Wednesday November 19th, at a presentation at CAW 1285 Hall Dennis Hull spoke on COPD (Chronic Obstructive Pulmonary Disease). Retirees, some with spouses were entertained by hockey legend (Ex-Blackhawk) Dennis Hull.
Dennis made the presentation entertaining with his wit and humour while at the same time stressing the seriousness of COPD and the fact that his sister had died from it.
Click here for more detailed
information on COPD
__________________



|
Health & Wellness: Spotlight on COPD
What is COPD ?
Chronic Obstructive Pulmonary Disease (COPD) is a devastating lung disease comprised of two major respiratory diseases – chronic bronchitis and emphysema
In 80% to 90% of cases, cigarette smoking is the principal underlying cause
COPD is Canada’s fourth leading cause of death
How Does COPD Develop?
Feeling of breathlessness at first generally thought to be due to age, being “out of shape”
People may experience:
Cough
Increased sputum
Chest colds or bouts of bronchitis that last for weeks
Breathlessness, wheezing
Difficulty with daily activities develops over time�
What Can We Expect?
Approximately 5 million Canadians currently smoke
Almost 84% of Canadians over 35 years of age with self-reported COPD were or had been smokers (91% of men; 77% of women) and almost 40% of those were still smoking
In 2004–05, the average length of stay in hospital for individuals aged 55 and over with COPD was 9.6 days
COPD is increasingly becoming a women’s health issue: more women than men are being diagnosed with the disease
|
Heart attack?
Don't drive - call 911
Making own way to ER may be fatal, study says
Sheryl Ubelacker
THE CANADIAN PRESS
Doctors have some simple advice for anyone with symptoms of a heart attack who needs to get to the hospital emergency room: leave the car in the garage and call 911.
Each year, thousands of Canadians experience the crushing chest pain and other telltale signs of a heart attack but choose to drive or be driven to their nearest ER instead of calling an ambulance. But doctors say that could be deadly.
"When it comes to heart attacks, every second counts," says Dr. Madhu Natarajan, a cardiologist at Hamilton Health Sciences. "The faster you get to the hospital, the faster you get treatment."
Natarajan presented a study to the Canadian Cardiovascular Congress in Toronto yesterday that found 40 per cent of people who went to the ER with heart attack symptoms had made their own way there.
Of the almost 500 patients studied, those who drove themselves or had a family member or friend take them were more likely to be younger, male, and with no history of heart disease.
"In general, people who are in the age range of 40 to 60 are more likely to drive themselves or find somebody to drive them to the hospital," Natarajan said in an interview.
"And also you see a lot of males between 50 and 70 who are married, their spouses drive them rather than them calling the ambulance."
He said people who come to hospital under their own steam can run into numerous delays – including traffic jams, difficulty finding the ER, lineups once they arrive and the time it takes to be triaged.
"We did see that people who came in by self (transport), their time to treatment was much longer," he said of the study.
And when it comes to a heart attack, there's an old saying that "time is muscle," meaning that heart cells can be irreparably damaged the longer they are starved of oxygen-rich blood. Calling 911 means quicker treatment: Paramedics are trained to recognize heart attack symptoms, can begin basic treatment and call ahead to prepare the ER.
Toronto Star |
LIST OF MAPLE LEAF RECALLED MEATS
Canadians are being told to dig through their fridges and freezers for any of the 220 Maple Leaf Foods products recalled by the Toronto-based company after test results
linked a plant in north Toronto to a nationwide listeriosis
Click here for a complete
list of recalled products (August 25, 2008)
Maple Leaf meat recall hits McDonald's, Mr. Sub

Health officials investigating whether
food poisoning, death are related
Paola Loriggio
STAFF REPORTER
Public health officials are investigating whether an outbreak of food poisoning that killed one person is linked to contaminated cold cuts produced at a north Toronto plant.
Seventeen people, 13 of them in Ontario, have fallen ill since June in an outbreak of listeriosis, a food-borne disease caused by listeria bacteria. An Ontario resident died of the illness.
Officials at the Public Health Agency of Canada say they know little about the outbreak or its victims, but are investigating a connection with a meat recalled by Maple Leaf Foods, which supplies companies including McDonald's and Mr. Sub.
The strain of listeria monocytogenes involved in the outbreak is the same one found in the meat, but that doesn't mean the two are related, said agency spokesperson Philippe Brideau.
The agency is asking victims to trace back what they have eaten in the past three months to see whether the outbreak is linked to the recalled cold cuts. It can take from two to 90 days for symptoms to appear, he said.
This morning, Maple Leaf Foods expanded a nationwide recall after bacteria was found in cold cuts produced at a Toronto plant that supplies companies including McDonald’s and Mr. Sub.
The Canadian Food Inspection Agency (CFIA) said the Maple Leaf meats – including sliced cooked turkey, roast beef, Bavarian smokes, corned beef, salami, ham and pepperoni – may be contaminated with the bacteria listeria monocytogenes.
The meats are sold under names including Schneiders, ML Sure Slice, Deli Gourmet, MSD, Burns, ML and FS. They include sliced turkey produced for McDonald’s and roast beef for Mr. Sub.
“These products have been distributed nationally, primarily to food service institutions such as restaurants, hospitals and nursing homes,” CFIA said in a statement. “In addition, these products may also be sold at retail and deli counters.”
None of the meat has been blamed for illnesses in humans, but “quite a large amount of product” is affected, said CFIA spokesperson Garfield Balsom.
In response, McDonald's has temporarily pulled the Turkey BLT sandwich from its Canadian menu, said spokesperson Louis Payette said.
Representatives of Mr. Sub and Maple Leaf could not be reached for comment this morning.
There are about 60 cases of listeriosis reported each year in Canada, but outbreaks are rare, Brideau said. About six have been reported since 1981, the first outbreak on record.
"It's not very common," he said. "It's not like salmonella. Most people have never heard about it."
Maple Leaf expanded the list of affected products after issuing a voluntary recall notice Sunday for two types of sliced beef sold under the Sure Slice name.
Although only a small batch products were found to contain listeria, Maple Leaf recalled dozens of products as a precaution and temporarily closed its Toronto plant to reassess food safety protocols there, according to a statement issued by the company.
Lists of the affected products are posted on the CFIA and Maple Leaf websites.
Consumers can also call Maple Leaf Consumer Foods at 1-800-568-5801 or CFIA at 1-800-442-2342 for more information.
Food contaminated with listeria monocytogenes may not look or smell spoiled. Consumption may cause listeriosis, a food-borne illness that can cause high fever, severe headache, neck stiffness and nausea.
Pregnant women, the elderly and people with weakened immune systems are particularly at risk. Infected pregnant women may experience only a mild, flu-like illness, however, infections during pregnancy can lead to premature delivery, infection of the newborn, or even stillbirth. |
Forget Viagra, eat watermelon

Betsy Blaney THE ASSOCIATED PRESS
LUBBOCK, Texas – A slice of cool, fresh watermelon is a juicy way to top off a barbeque and one that researchers say has effects similar to Viagra – but don't necessarily expect it to keep the fireworks all night long.
Watermelons contain an ingredient called citrulline that can trigger production of a compound that helps relax the body's blood vessels, similar to what happens when a man takes Viagra, said scientists in Texas, one of the top producers of the seedless variety in the U.S.
Found in the flesh and rind of watermelons, citrulline reacts with the body's enzymes when consumed in large quantities and is changed into arginine, an amino acid that benefits the heart and the circulatory and immune systems.
"Arginine boosts nitric oxide, which relaxes blood vessels, the same basic effect that Viagra has, to treat erectile dysfunction and maybe even prevent it," said Bhimu Patil, a researcher and director of Texas A&M's Fruit and Vegetable Improvement Center. "Watermelon may not be as organ-specific as Viagra, but it's a great way to relax blood vessels without any drug side effects."
Todd Wehner, who studies watermelon breeding at North Carolina State University, said anyone taking Viagra shouldn't expect the same result from watermelon.
"It sounds like it would be an effect that would be interesting but not a substitute for any medical treatment," Wehner said.
The nitric oxide can also help with angina, high blood pressure and other cardiovascular problems, according to the study, which was paid for by the U.S. Department of Agriculture.
More citrulline – about 60 per cent – is found in watermelon rind than in the flesh, Patil said, but that can vary. But scientists may be able to find ways to boost the concentrations in the flesh, he said.
Citrulline is found in all colours of watermelon and is highest in the yellow-fleshed types, said Penelope Perkins-Veazie, a USDA researcher in Lane, Okla.
She said Patil's research is valid, but with a caveat: One would need to eat about six cups of watermelon to get enough citrulline to boost the body's arginine level.
"The problem you have when you eat a lot of watermelon is you tend to run to the bathroom more," Perkins-Veazie said.
Watermelon is a diuretic and was a homeopathic treatment for kidney patients before dialysis became widespread.
Another issue is the amount of sugar that much watermelon would spill into the bloodstream – a jolt that could cause cramping, Perkins-Veazie said.
Patil said he would like to do future studies on how to reduce the sugar content in watermelon.
The relationship between citrulline and arginine might also prove helpful to those who are obese or suffer from type-2 diabetes. The beneficial effects – among them the ability to relax blood vessels, much like Viagra does – are beginning to be revealed in research.
Citrulline is present in other curcubits, like cucumbers and cantaloupe, at very low levels, and in the milk protein casein. The highest concentrations of citrulline are found in walnut seedlings, Perkins-Veazie said.
"But they're bitter and most people don't want to eat them," she said.
thestar.com
****************
Ignorance is not bliss

Avoiding prostate tests because you're afraid of hearing bad news could be deadly mistake
Paul Irish - Toronto Star
Don't be an ostrich!
You know who you are. Are you the guy who hides his head in the sand refusing medical tests or examinations because he's scared he may be sick?
As ridiculous as it sounds, there are a lot of those frightened birds out there.
Colin Graham, 74, admits he had a touch of the ostrich in him.
But he still had enough sense to listen to his doctors – and he's glad he did.
In early 2005, Graham's family doctor felt an irregularity in his prostate gland while performing a digital rectal exam.
He sent Graham to Sunnybrook's Odette Cancer Centre for a PSA test, which proved normal.
But because of other factors – Graham's age and the facts that cancer runs in his family and his prostate gland was irregular – Sunnybrook doctors determined he had a high risk of having prostate cancer.
A biopsy proved them right, and the prostate was removed.
"I didn't feel the slightest bit sick ... I didn't know I had it," Graham says. "Men should take full advantage of anything that will help them detect the cancer. My PSA was normal, but look what happened."
Dr. Robert Nam, a urological oncologist at Sunnybrook, was able to detect Graham's prostate cancer thanks to a nomogram, which classified him as a high-risk patient even though his PSA levels were normal.
A nomogram is a statistical model that determines the threat of cancers or disease based on known risk factors.
Sunnybrook's model – called the Prostate Cancer Risk Calculator – takes just minutes to determine the level of risk, based on age, family history, ethnicity, urinary symptoms, PSA, free/total PSA ratio and rectal exam results.
It's the first nomogram to use all known risk factors for prostate cancer, and has already proven to be more reliable than conventional cancer screening.
Nam says a PSA test may not detect smaller cancers, but once other markers are taken into account, the nomogram can identify patients at a high enough risk to warrant a biopsy. Although he says the PSA number will always be important, it is more useful when used in context with as much information about the patient as possible.
To see how the nomogram works, go to the website at prostaterisk.ca and click on the link to the risk calculator. However, it is best used in consultation with a family doctor.
Sunnybrook researchers based the nomogram on 3,108 Canadian men (all of whom had abnormal PSA values or rectal exam results), along with another group of 408 volunteers with normal PSAs.
All of the men underwent prostate biopsies.
Of the main group, 42 per cent were diagnosed with prostate cancer.
Of the 408 with normal PSAs, 24 per cent were diagnosed with prostate cancer.
Further evaluation of the nomogram is underway, through a multi-institutional cross-Canada study group of another 5,000 men.
"In addition to helping men avoid unnecessary biopsies, the risk calculator better detects prostate cancer at an earlier, more curable, stage," Nam says.
"And it helps identify high-risk patients who may need to make immediate dietary and lifestyle changes and need repeat biopsies."
********************************
Shower curtain health warning
PVC vinyl leaching pollutants into air, study finds
Huixia Sun
STAFF REPORTER
Some shower curtains may be hazardous to your health, according to a new study released yesterday.
As many as 100 harmful chemicals are released into the air from PVC shower curtains, posing risks to human health and the environment, says the study, released jointly by the U.S.-based Center for Health, Environment and Justice, Canada-based Environmental Defence, and the Canadian Environmental Law Association (CELA).
Researchers purchased polyvinyl chloride (PVC) shower curtains from five American retailers. In laboratory tests they were found to contain chemicals including volatile organic compounds (VOCs), phthalate, organotins and metals. Several chemicals found in the curtains are considered a human health concern under the Canadian Environmental Protection Act, but are not regulated, according to the report.
Toxic chemical off-gassing may contribute to respiratory problems, and damage the liver, central nervous and reproductive systems, said the report, titled "Volatile vinyl: the new shower curtain's chemical smell."
Pregnant women and children are particularly vulnerable, and heat or humidity can increase the release of chemicals, said the report.
"Not only are vinyl products contaminating our indoor air, but they release toxic dioxins during manufacturing and incineration," said Theresa McClenaghan, CELA's executive director. "The federal government has a window of opportunity to proactively regulate these chemicals with a major bill before Parliament to amend the federal Hazardous Products Act."
Environmental Defence and CELA are urging Ottawa to ban PVC in shower curtains and calling on manufacturers and retailers to switch to safer products such as cotton shower curtains. They are also urging expanded labelling rules. .
Responding to the study yesterday, a council of the Canadian Plastics Industry Association denied that the chemicals in the curtains were dangerous to consumers.
"Just because a chemical has been detected does not mean that it's harmful," said the director of the Vinyl Council of Canada, Marion Axmith, in a news release.
Calling the report "simple scaremongering," she said vinyl shower curtains had been in use "for decades with no reported incidents of harm."
With files from Nick Kyonka
**********************************
Toronto Star
Middle-aged spare tire
linked to Dementia

THE CANADIAN PRESS
Carrying a spare tire on the abdomen is known to significantly boost the risk for diabetes and cardiovascular disease, but new research suggests excess belly fat in middle-age also may contribute to Alzheimer's and other forms of dementia later in life.
In fact, a long-term study of more than 6,000 people found that those with the highest amount of abdominal fat in their 40s had about triple the risk of developing dementia than those with the lowest amount of fat around their mid-sections.
Having a bulging belly boosted the risk of dementia regardless of whether participants had normal weight overall or were overweight or obese, as measured by body mass index (BMI), said principal investigator Rachel Whitmer, a research scientist at Kaiser Permanente, a non-profit U.S. health plan that conducted the study.
Furthermore, the increased risk of Alzheimer's and other dementias existed independently of other health conditions, including diabetes, stroke and heart disease – and the effect did not vary by race or gender, Whitmer said from Oakland, Calif.
The study, published Thursday in the journal Neurology, found that those who were overweight by BMI standards and also had a pot belly were 2.3 times more likely to develop dementia than people with a normal weight and abdominal profile, she said.
Those who were both obese and big around the middle were 3.6 times – or a whopping 260 per cent – more likely to develop dementia than those of normal weight and belly size. That compares to an 80 per cent higher risk for people who were overweight or obese but without so-called beer gut.
"So there's two messages here," Whitmer said. "The first message is that if you are normal (weight) and you have a large belly, your risk for dementia was about the same as those who were overweight or obese who didn't have a large belly."
"Now, if you are overweight or obese and you have a large belly, your risk really goes up."
"So this really nicely shows that the effect of the large belly was above and beyond the effect of body mass index and, in particular, the magnitude of the effect of the large belly got greater as you weighed more."
The study involved 6,583 people in northern California, aged 40 to 45, who had their abdominal fat measured between 1964 and 1973 and whose health records were followed over time. An average of 36 years later, when participants were in their 70s, 16 per cent had been diagnosed with dementia.
Whitmer said the kind of fat that settles in the belly, known as visceral fat, has a different makeup and actions in the body than the type of fat packed on elsewhere, called subcutaneous fat.
"And fat biologists know, that visceral fat, it is more lively, it is more toxic, it is more metabolically active," said Whitmer. ``It secretes a lot of hormones and inflammatory compounds."
While only speculating, she suggests one or more of these inflammatory substances may be able to cross into the brain and cause damage – just as they may do to blood vessels and organs like the heart and pancreas.
"It's not a causal study, it's not a mechanistic study," she said. "But I think our findings suggest there is a pathway going on that is something intrinsic to that belly size, to that belly fat, because we did take into account other diseases that are highly correlated with belly size and highly correlated with dementia."
Dr. Jean-Pierre Despres, a specialist in obesity and cardiovascular disease at Laval University, said he is not surprised to see a relationship between excess abdominal fat and dementia.
"Obviously this is an association and you don't want to speculate too much on the mechanism behind such associations," Despres said Wednesday from Quebec City.
"But if you think about the consequences of abdominal obesity, of having fat at the wrong place, we know that having too much abdominal fat is associated with what I call a minestrone soup of abnormalities, increasing the risk of Type 2 diabetes, but also increasing the risk of cardiovascular disease."
"Now I'm learning today that on top of the risk of heart disease, the risk of diabetes, this is one more complication to add to the expanding list, which makes this extremely interesting," said Despres, who was not involved in the study.
While more research is needed to pin down exactly how having a paunch might affect the brain, he said the study provides more evidence that having fat in the wrong place is detrimental to health.
"It's not a matter of how fat you are, it's where the excess fat is located," said Despres, noting that a portly girth (roughly more than 94 centimetres in men and 80-plus centimetres in women) and elevated blood fat (triglycerides) suggests a build-up of visceral fat.
Dr. Cheryl Wellington, an associate professor of pathology and laboratory medicine at the University of British Columbia, called the Neurology paper a "landmark study that strengthens the connection between metabolic disturbances and the onset of dementia."
"What is really important about studies like this is that it actually provides people with things that they can do to help lessen their risk of dementia in old age," she said from Vancouver.
"Taking good care of yourself in midlife is probably the biggest thing that you can do to preempt dementia as much as possible later. So when you're in your 30s and 40s and 50s, make sure you've got diet and exercise under control."
Whitmer agreed that having too much visceral fat may be risky, but the good news is it's a risk that can be modified.
"It is actually less stubborn than the subcutaneous fat, so you can get rid of that fat with exercise and with diet."
thestar.com
*******************************
Two stand-outs for those seeking pre-summer tan

Peggy MacKenzie
TORONTO STAR
Here comes the sun and I say it's time to get our tan on. Literally. No frying for us under a sun lamp or following the sun in our backyards. With the self-tanning products on the market, broiling on the beach to achieve that bronze look is so passé.
Self-tanning products are safe, Toronto dermatologist Dr. Cheryl Rosen writes in an email, "as long as people don't rely on them to be sunscreens." All the self-tanning products warn consumers to put sunscreen over top of the tanner if going out into the sun. Other things to keep in mind:
If you're sensitive to smells, take a sniff at the store. Some had no smell while others lasted throughout the day.
All tanners warn to spread evenly but sparingly over knees, knuckles, toes and ankles. This is easier to do in theory.
They also warn you about ruining your clothes if you don't wait long enough for the product to dry. All tanners varied wildly on drying time.
Vicky, at the Shoppers Drug Mart at Union Station, says to exfoliate before applying the tanners and moisturize after (if needed).
We tested legs for this column but some of the tanners advertise that they're for the whole body, including faces. Check the label to make sure.
All five of Test Drive's pasty-white testers complained there weren't enough instructions even though an error in application has serious consequences to your body and clothes.
All the tans were intact after shaving, although the Marcelle tester found the tan "bled" a little onto the razor but there was no change in the colour on her legs.
To the bronzed beauties in the photo – Gale, Deb, Libby and Jane – a big thank you. I was also a tester.
Clarins Self-Tanning Instant Gel
    Cost: $35 Cost: $35
Size: 125 mL
Drying Time: 15 to 20 minutes
Moisturizer: Yes.
Scent: Yes. Pleasant
Libby had a lot of time to contemplate this gel after the first application. She read the minimal instructions, washed her hands and nails thoroughly after use, and then waited for three hours while it dried. "I think I applied it with too heavy a hand," she jokes, since the product normally dries in under 20 minutes. "It smells wonderful – like every Clarins product I've ever used," she says, adding that this tanner was even a great moisturizer. "(It) got rid of the alligator-skin look my legs usually have all winter." She liked the colour and, unlike the rest of us, there were no splotches after her first try.
Roc Minesol Bronze Self-tanning lotion
Johnson & Johnson
   
Cost: $19
Size: 100 mL
Drying Time: 30 minutes
Moisturizing properties: Yes
Scent: Yes. Pleasant
Jane used this lotion six times over the two weeks before the last photo shoot and her legs have the look she normally has in the summer. She waited a minimum of one hour before getting dressed but had to dodge her dog who tried for a quick ankle lick. The minimal instructions made it difficult "to determine how, how much, and where to apply." The white lotion was a good consistency and coated evenly with almost no aroma. Dry skin areas, though, absorbed it quickly and then developed a yellowish hue. Immediately after applying, Jane noticed a slight tingling sensation and a slight "suntan lotion" smell that was clean and fresh. That's when the dog moved in. Like Clarins and Biotherm, a rounded tablespoon was enough for one application. It absorbed well, with no stickiness.
Neutrogena Build-a-Tan
   
Cost: $13.99
Size: 200 mL
Drying Time: 5 minutes.
Moisturizing properties: Yes.
Scent: Yes. Unpleasant chemical smell that lasted all day.
I used this lotion daily for five days before the last photo shoot and every other day for two weeks before that. The colour appeared natural to me, not orangey, and does slowly build over time. Applying the lotion was easy from the pump but, because I feared having a two-toned result on my ankles and knees, I applied sparingly on those areas and still created that look anyway. To ensure even coverage, you'd have to use this product for at least a week before showing your legs to the world. I found it reassuring that the tan built over time, since there's too much room for error with an instant tan. The drying time was minimal and, to check if the colour bled, I wore white socks and never noticed any colour on them. This tanner was the cheapest of the lot but worked very well once I got into the swing of it. Now that I've stopped for three days, however, my tan isn't as even.
Biotherm Sun Tan Gel Beautiful Legs
  
Cost: $30
Size: 150 mL
Drying Time: 45 minutes
Moisturizer: No.
Scent: Yes. A "chemical" smell
Gale likes that the gel is bronze-coloured for application, since it was easy to see the coverage against her white legs. After one application, she did see a slight bronze colour, but also streaks. Getting the product to "feather" or fade on Gale's feet was hard and she had a "start" line that looked unnatural. The colour darkened after the second application and the streaking was minimized. Her knees were another hard area to tan: "I had two large circles of dry skin." When the tanner dried, Gale's skin "felt a little tight, like it contracted when it dried. I had to moisturize big time." The odour was neither pleasant nor unpleasant, but it did have a "chemical" smell. Gale wished there was an insert "explaining if it would stain, how long I should wait before I dressed, if I could use it on my arms or torso." A towel did get stained but the stain washed out.
Marcelle Tinted Self-Tanning Gel-Cream
  
Cost: $12.95
Size: 100 mL
Drying Time: 5 minutes
Moisturizer: No
Scent: Yes. The bottle says "perfume free" but Deb smelled "molasses with a chemical smell like the paint in my new kitchen but with a vaguely sweet undertone."
Deb used the product almost daily but her legs didn't get very dark. The gel spread easily and she was careful not to spread it too thick on her knees and ankles but noticed "the more I used it, the more speckly my legs looked." Also, she says she walks into things a lot – "I always have bruises on my shins" – and the bruises turned a darker colour than the rest of her leg.
She didn't notice any staining on her clothing but always waited at least five minutes before getting dressed. The tanner is not a moisturizer, and Deb noticed that her skin had a "papery" texture. She used a moisturizer after application.
Deb wonders about the safety of using self-tanners, with all the chemicals listed. Instead of competing with a beach tan in the summer, she'll aspire "to an 18th-century standard of beauty."
************************************
A Guide to Diabetes
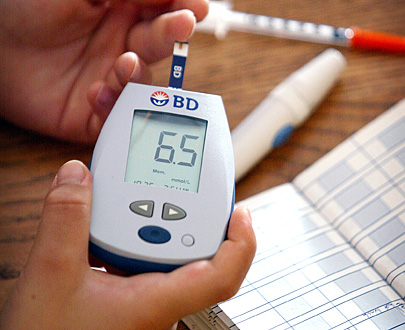
What is diabetes?
Diabetes is a disease in which blood glucose is above normal levels. Our bodies convert food into glucose, the main source of fuel for our bodies. The pancreas makes a hormone called insulin, which helps glucose get into the cells of our bodies.
With diabetes, the pancreas either produces little or no insulin, or the cells do not respond appropriately to the insulin that is produced. This causes sugar to build up in the blood, overflow into the urine and pass out of the body.
As a result, blood sugar levels can drop too low, leading to a coma, or sustained elevated blood sugars can lead to damage of major organs such as the kidney and heart. The disease also puts people at risk for blindness and lower-extremity amputations due to wounds that do not heal properly.
DID YOU KNOW?
Rising numbers: More than 2 million Canadians have diabetes, with that number expected to rise to 3 million by 2010. The World Health Organization estimated in 2000 that more than 177 million people worldwide have diabetes. By 2025, it will top 300 million.
Complications: About 80 per cent of people with diabetes will die as a result of heart disease or stroke.
Premature deaths: Diabetes is a factor in the deaths of about 41,500 Canadians each year. Canadian adults with diabetes are twice as likely to die prematurely than those without diabetes.
Shortened life: Life expectancy for type 1 diabetics may be shortened by as much as 15 years.
Medical costs: A person with diabetes incurs medical costs that are two to three times higher than those without diabetes. A diabetic can face direct costs for medication and supplies ranging from $1,000 to $15,000 a year.
Health-care system: Based on a U.S. study, diabetes and its complications cost the Canadian health-care system an estimated $13.2 billion every year. By 2010, it's estimated these costs will rise to $15.6 billion a year and, by 2020, $19.2 billion a year.
Cutting risks: In a large study, people at risk of type 2 diabetes cut that risk 58 per cent by exercising moderately for 30 minutes a day and by losing 5 to 7 per cent of their body weight. In those over 60, the risk was cut by almost 71 per cent. Other studies have shown similar results.
Type 1
Definition: Previously called insulin-dependent diabetes mellitus (IDDM) or juvenile-onset diabetes, type 1 is an autoimmune disease in which the body makes little or no insulin.
Risk factors: Type 1 develops most often in children and young adults before age 30, although it can appear at any age. There is no known cause and, thus, no way to prevent it. It is not caused by consuming too much sugar.
Symptoms: Usually develop over a short period, although cell destruction can begin years earlier. Symptoms include increased thirst and urination, constant hunger, unexplained weight loss, blurred vision, extreme fatigue, tingling or numbness in hands or feet, very dry skin, sores that are slow to heal and more infections than usual. Those affected do not necessarily show symptoms. Risk factors are less well defined for type 1 than for type 2, but autoimmune, genetic and environmental factors are involved.
Treatments: A person who has type 1 diabetes must take insulin daily to live. Lifestyle changes such as healthy eating and increased physical activity are basic therapies. Blood glucose levels must be closely monitored through frequent blood glucose testing.
Complications: Early heart disease, amputation, stroke, kidney failure, nerve damage, blindness.
Type 2
Definition: Previously called non-insulin-dependent diabetes mellitus (NIDDM) or adult-onset diabetes, type 2 is the most commonly diagnosed type of diabetes. With type 2 diabetes, the body can't use the insulin it makes.
Risk factors: Associated with those age 40 or older, obesity, family history of diabetes, high blood pressure, abnormal cholesterol levels, schizophrenia, polycystic ovary syndrome, acanthosis nigricans (darkened patches of skin), previous history of gestational diabetes, history of giving birth to a baby more than 9 pounds, physical inactivity and ethnicity (Aboriginal, Hispanic, Asian, South Asian, or African descent); type 2 is increasingly being diagnosed in children and adolescents.
Symptoms: Develop more slowly and may include fatigue or nausea, frequent urination, unusual thirst, weight loss, blurred vision, frequent infections and slow healing of wounds or sores; or there can be no symptoms.
Treatments: Healthy eating, physical activity and blood glucose testing are basic therapies. Many require oral medication, insulin or both to control blood glucose levels.
Complications: High blood glucose levels over a long period can cause blindness, heart disease, kidney problems, amputations, nerve damage and erectile dysfunction.
Gestational
Definition: Glucose intolerance, but with first onset during pregnancy.
Risk factors: It only affects women during pregnancy and usually disappears after pregnancy. Risk factors include a history of gestational diabetes, age over 35, obesity, a history of polycystic ovary syndrome, hirsutism (excessive hair growth in women), acanthosis nigricans and being a member of a population considered to be at high risk for diabetes.
Symptoms: The Canadian Diabetes Association's 2003 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada recommend that all women be screened between 24 and 28 weeks gestation using a glucose tolerance test. For those with multiple risk factors, this testing should be done during the first trimester, then again during the second and third trimesters, even if the first test is negative.
Treatments: Similar to managing type 2 diabetes, nutritional therapy is recommended to achieve euglycemia or blood-glucose balance. It's important to ensure appropriate weight gain, but not weight loss, and adequate nutritional intake for mother and baby. If reductions in blood glucose do not reach the recommended levels within two weeks after eating and exercise adjustments, then certain types of insulin can be safely used in pregnancy.
Because women with a history of gestational diabetes risk developing type 2 diabetes later in life, a follow-up blood glucose test is recommended within six months of childbirth. In addition, it is recommended that women breastfeed to reduce the risk for subsequent diabetes in the baby. Women should be screened regularly for type 2 diabetes.
Complications: Babies born to mothers with gestational diabetes may be macrosomic (severely obese). This poses a risk of trauma to mother and child during childbirth.
Macrosomic babies have a higher risk of severe breathing problems and hypoglycemia (severely low blood glucose levels) after birth. They are also at higher risk for potential long-term obesity and glucose intolerance. Generally, glucose levels in women who have had GDM return to normal.
However, these women do face an increased risk of developing type 2 diabetes later in life.

LIVING WITH DIABETES
(CLICK HERE)
------------------------------------------------------------------------------Sources: Canadian Diabetes Association, Centers for Disease Control, National Diabetes Information Clearinghouse / Compiled by Marian Traynor and Peggy Mackenzie, Toronto Star Library.
***********************************************
Study finds antidepressants no better than sugar pills
Feb 27, 2008 Toronto Star
Study: Four of the most commonly prescribed antidepressants, including Prozac, work no better than placebo sugar pills to help mild to moderate depression, says a study published in PloS (Public Library of Science) Medicine. Irving Kirsch of the department of psychology at Hull University in England and colleagues in the U.S. and Canada compared trial results for patients taking a sugar pill with those given the antidepressants fluoxetine (Prozac), paroxetine (Seroxat), venlafaxine (Effexor) and nefazodone (Serzone). They found that patients felt better but those on placebos improved as much as those on the drugs. The only exception: the most severely depressed did better on the drugs.
Method: Using freedom of information rules, researchers obtained a full set of trial data from the U.S. Food and Drug Administration, including results the drug companies had chosen not to publish.
Background: Prozac has been used by 40 million patients since 1988.
Claim: "There seems little reason to prescribe antidepressant medication to any but the most severely depressed patients, unless alternative treatments have failed to provide a benefit," Kirsch says. Alternatives include talk therapy.
Caveat: Patients are strongly advised not to stop taking medication without consulting their doctor. "This analysis has only examined a small subset of the total data available while regulatory bodies around the world have conducted extensive reviews and evaluations of all the data available," says GlaxoSmithKline, which makes Seroxat. Eli Lilly, maker of Prozac, also defended research showing the antidepressant is effective.
*********************************
GLOBAL EPIDEMIC
TheStar.com | Health | TB’s deadly comeback
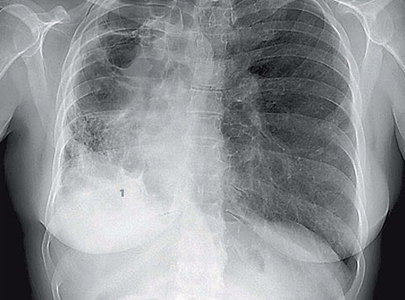
Toronto, with its growing immigrant population, will likely see an increase of deadly, contagious tuberculosis, experts say. The current system simply couldn't handle an outbreak, but the province has yet to make the changes required to protect citizens
Megan Ogilvie
Health Reporter
At first, Lynda thought it was a cough like any other: a dry hack that rattled her chest from time to time. Nothing to be bothered about.
But soon the tickle was accompanied by a high fever, unrelenting fatigue and a deep, aching pain in her right lung.
Worried, the 41-year-old mother went to see her family doctor in Newmarket. She told him about the persistent cough, that she had inexplicably lost 20 pounds in the spring, and how she felt dark shadows of depression slowly creeping over her.
He advised her to work fewer hours and stop smoking, and he sent her home with stronger asthma medication. But months passed, and Lynda, who continued to see her doctor, kept getting weaker and weaker, until one day she was unable to climb a flight of stairs.
"That was a scary feeling because I knew something was not right," recalls Lynda. "In my head I heard a voice. It said, I think I'm dying."
She was.
Hordes of tuberculosis bacteria were living in her lungs, thriving and multiplying, steadily destroying the delicate tissues.
But since many Canadians consider tuberculosis a thing of the past, Lynda's family doctor misdiagnosed the deadly disease for months. Since she got her diagnosis two years ago, she has told few people, for fear of being ostracized – which is why she asked the Star not to use her last name.
Experts say few family doctors know the singular signs of tuberculosis any more. And few patients nowadays consider that they might be suffering from a disease that once killed thousands of Canadians every year, and then seemed to vanish.
Yet tuberculosis hasn't disappeared from our neighbourhoods. In Toronto, more than any other city in Canada, there is still an undercurrent of disease. About one-quarter of the country's TB cases are here – there are currently about 1,600 active cases in Canada and 400 in Toronto – and experts expect the incidence to rise as immigration swells from countries where TB is epidemic.
Despite those concerns, Ontario is the only TB-afflicted province without a centralized system of tuberculosis clinics. Right now, many Ontario TB patients are seen by doctors who have little experience with the disease, rather than specialists.
That means patients are being diagnosed too late and given less-than-aggressive treatment – and so are more likely to develop resistance to the antibiotics, to have permanent lung damage, to relapse later on in life, and even to die. They are also more likely to pass on the disease to the people around them.
Experts also say the current system is only just keeping up with demand and would be woefully inadequate if a TB outbreak hit the city.
"Many developing countries are doing a better job of managing TB than we do," says Dr. Michael Gardam, chief of infection control at the University Health Network and head of the tuberculosis clinic at Toronto Western Hospital.
Tuberculosis is a highly infectious disease that is passed from person to person when an infected person coughs or sneezes and spreads bacteria into the air. More than one-third of the world's population is infected with the TB bacillus – of them, about 10 per cent will go on to develop full-blown TB, which then becomes infectious (according to Dr. Kamran Kahn, a tuberculosis expert at St. Michael's Hospital, close to a million Canadians have latent tuberculosis). Close to 2 million people will die from it this year.
In recent years, some strains have become resistant to our best antibiotic treatments, making what is often a curable disease much more difficult – and sometimes impossible – to treat. The World Health Organization says extremely drug-resistant tuberculosis, or XDR-TB, is one of its top concerns and calls it a grave public health threat.
The threat of drug resistance first emerged in Tugela Ferry, a rural town in KwaZulu-Natal province in South Africa, when an outbreak of XDR-TB killed 52 of 53 infected patients. XDR-TB has been reported in 41 countries, including Canada.
Concern about drug-resistant tuberculosis proliferating in North America came into focus last May and June when infected Atlanta lawyer Andrew Speaker ignored public health warnings and endangered fellow passengers when he took commercial flights to his wedding in Greece and then returned to North America via Montreal.
Meanwhile, it's the rampage of tuberculosis outside our borders that has Toronto TB experts so worried. The WHO warns, "TB anywhere is TB everywhere." And especially with the surge in global travel and the role of the GTA as a hub for new immigrants, this city may be particularly vulnerable.
"Toronto reflects the world, and the world is having an epidemic of TB," says Gardam. "If the world has a problem, then we have a problem."
Up until the early 1980s, Ontario did have a centralized system of tuberculosis clinics managed by each region's public health unit and run by the province. But as infection rates fell, officials assumed the disease would eventually be eliminated, and the system was dismantled.
"It seemed like infectious diseases would disappear from the planet," says Dr. Elizabeth Rea, an associate medical officer of health for Toronto Public Health's TB prevention and control program. "They haven't. Particularly for Toronto. Our rates are driven by what is happening outside the city ... TB is not going to disappear from Toronto as long as we are an immigration centre. We need to plan for cases to continue to arrive here and to be able to deal with them at the highest level of care."
Toronto's TB rate has slowly been slowly going down for the past 10 years but, cautions Rea, "Every single jurisdiction that has cut back on TB control has had a resurgence."
New York City offers the most striking object lesson. In the early 1990s, after the city had repeatedly cut spending on TB control, an outbreak swept through the most vulnerable communities – the homeless, working poor crammed into tight living quarters, people with immune systems beaten back by HIV. By 1992, there were 3,811 new cases of TB, up from 1,307 cases in 1978, the first year the city kept statistics.
"It was a massive, heartbreaking outbreak," says Rea. "It took years and millions and millions of dollars to get it under control."
According to The New York Times, the city spent $40 million on tuberculosis control in 1993, in the midst of the epidemic, compared to $4 million in 1988.
Toronto has seen it's own mini-outbreaks of TB in the shelter system. In 2001, Joseph Teigesser died of tuberculosis while living in a city shelter during a 17-month-long outbreak that also infected 15 other homeless people.
A 2004 inquest into Teigesser's death made 13 recommendations, primarily to the provincial government, for reducing TB transmission among the homeless. One of them was for the Ministry of Health to establish a centralized clinic system for TB management, funded 100-per-cent by Queen's Park.
Since 2000, at least seven reports, including one by the Ontario Medical Association, have recommended a centralized model of TB care. In 2005, the ministry convened a task force of tuberculosis experts to outline how such a system could be implemented. Eighteen months ago the task force submitted its 25-page report – endorsed by the Lung Association, the Homeless and Underhoused Community Advisory Panel and the Tuberculosis Prevention and Control Program of the Public Health Agency of Canada – but still hasn't received a response from the province.
According to ministry spokesperson Andrew Morrison, the ministry supports the proposed model for developing a centralized clinic system in Toronto and is currently reviewing the task force's proposal.
According to the provincial task force, the current fragmented system means TB patients are not being managed properly as set out by Canadian Tuberculosis Standards, a book on prevention and treatment published by the Public Health Agency of Canada and the Lung Association. The task force also says they are at higher risk of dying or developing drug resistance and are staying sick longer, which increases their likelihood of spreading the disease.
Right now, there are four tuberculosis clinics in Toronto – at Toronto Western, St. Michael's and Sick Kids hospitals and at West Park Healthcare Centre, the only hospital in the province to offer long-term in-patient care for TB patients. All these facilities get funding from their respective hospital foundations. There are no such clinics in 905 areas.
Kamran Kahn of St. Michael's Hospital says it's becoming more and more challenging for the four clinics to keep up with demand, because patients are arriving with complex health and social issues. And he points out that three of the clinics are downtown and hardly accessible to the many immigrant patients who live east, west and north of the city.
The 2006 task force, which Kahn was a part of, highlighted the immediate need for two additional TB clinics, one in Etobicoke and one in Scarborough, a neighbourhood that sees, on average, one-third of the city's active patients.
What all of this means, says Kahn, is that family physicians in the GTA have to pick up the slack. In 2002, he points out, there were 178 physicians managing TB cases in southern Ontario, and few doing it well since almost two-thirds had managed less than one TB case per year.
These front-line health-care workers, used to diagnosing diabetes, heart disease and the other chronic diseases confronting modern-day North America, can miss the cluster of symptoms that spell tuberculosis – a constant cough, unexplained weight loss, night sweats, a general feeling of malaise. Especially when the patients do not come from prisons, homeless shelters and the other overcrowded settings where TB usually emerges.
In a 2006 study published in the Canadian Medical Association Journal, Kahn and Gardam found patients who were treated by TB-experienced physicians were less likely to die than those treated by inexperienced physicians.
Just as cancer patients are referred to cancer clinics, experts say tuberculosis patients need to be managed by specialists. Kahn says this is particularly true for complicated TB cases, including patients who are new to the country and who may not speak English and those who have other health problems, such as HIV or mental illness. More than 90 per cent of TB patients in Toronto are foreign-born.
Most days, Lynda can hardly believe she has tuberculosis. It's been two years since she was diagnosed with the disease, and she's not sure if she'll ever get her old life back.
At 43, the vivacious mother in York Region wants to be out playing with her two young daughters, not confined to a couch because her lungs have been ravaged by TB. Even now, a cough could turn into a phlegm-filled fight for breath.
"It's changed my life so much," she says. "I'll have a couple of good days, then some bad days. Every morning I cough, every morning I gag, every morning I retch. It hurts to laugh. I can't run. I was always a hard-working person, I can try to go-go-go, but ... "
Lynda is waiting to hear whether her right lung, which has been almost completely destroyed by the disease, will have to be removed.
"I guess if it was caught sooner, maybe it wouldn't have been so bad," she says.
Gardam, who now treats Lynda at his clinic at Toronto Western, confirms that she would be well now if she had got proper care from the start. Not only was Lynda misdiagnosed by her family doctor, but when she finally got a proper diagnosis six months later, the community hospital gave her the wrong regime of antibiotics.
"There is no doubt, the earlier you catch it, the better you do," he says. "In general, (Lynda's) case is a very common story for us."
Lynda never wanted to be an example of what is wrong with Ontario's current tuberculosis care system. But that is exactly what she has come to be. She still doesn't know where she got infected, though there's some evidence she got it at the factory where she worked for three years.
Lynda pauses to cough, making a gurgling sound, and then goes on.
"It's not just a Third World problem, I don't think," she says. "It's coming back here ... People need to be educated about tuberculosis ... It's not a dead disease."
******************************************
The truth about MSG

MSG, or monosodium glutamate, is the heavyweight champion of flavour enhancers the world over.
It was discovered in seaweed. A century later, monosodium glutamate
MSG –is the heavyweight champion of food additives. It's also a villain.
What else do you sprinkle on steak that's the subject of conspiracy theories?
Murray Whyte
Staff Reporter
An innocent question, asked recently at a very popular, very established Chinatown eatery that shall remain nameless: "Do you use MSG?"
The answer? "We always put a little bit," the cheery waiter replies. "If you want more, we can put more."
Say what? To some ears, the helpful-seeming offer would sound much like choosing to endure a more severe beating if the first wasn't painful enough. Indeed, to say that MSG, or monosodium glutamate, far and away the heavyweight champion of flavour "enhancers" the world over, has a checkered history is something of an understatement.
This year, it enjoys the dubious distinction of its centenary as an officialized food additive. Since its intitial isolation in 1908 by a Japanese chemist, Kikunae Ikeda, it's become a food industry staple, and along the way, hailed as both a revolutionary innovation and a despised symbol of callous quasi-food profiteering.
Either way, it's been a prevalent ingredient in the North American diet for 60 years (the brand of MSG called Accent was introduced here in 1947), embraced in the post-war "better living through chemistry" era as a cheap, easy way to boost flavour in any number of packaged or canned foods.
And for almost as long, it's been maligned, fairly or unfairly, as a chemicalized toxin blamed, according to Health Canada, for migraines, hypertension, nausea and chest pain. More extreme – and often unproven – accusations have linked MSG to obesity, diabetes and liver inflammation. The Times of India – and, curiously, nowhere else – reported just this month that the Netaji Subhas Chandra Bose Cancer Research Institute, an institution without a website, apparently, had concluded in a report that MSG causes cancer.
Careful, though. In the haze of MSG hysteria, dark conspiracies and gruesome consequences are the norm (in the same report, the newspaper claimed that MSG had been declared unsafe by the World Health Organization in 2004, but the report could not be located; meanwhile, a 2005 WHO report says MSG has "no adverse effects.")
Such is the potent mythos of the great villain of all food additives. One thing that's indisputable: MSG's continued – and in some cases, growing – presence in all our diets. Despite the organic food craze blossoming in some circles, MSG is doing quite nicely, thank you. According to the Food Ingredient News, a specialized (to say the least) trade publication, MSG consumption globally was increasing by 2.5 per cent per year.
Granted, more than 80 per cent of the consumption is in Asia, and growth, specifically in China. There, MSG, in its raw form, a powdered, white crystalline substance, is left on restaurant tables like salt or pepper for customers to administer to their liking. And it's more pervasive in the North American diet than ever before. MSG may be additive-non-grata here, but keep your eyes peeled: Hydrolyzed protein, autolyzed yeast extract and dozens of others – all contain MSG.
It was in 1968 when the New Hampshire Journal of Medicine coined the somewhat politically incorrect term "Chinese Restaurant Syndrome" for the apparent prevalence of MSG in Asian foods and the apparent symptoms its consumption could cause. You would have expected MSG to wither away. The furor prompted Chinese restaurants all over North America to display an exculpatory sign in their window: "NO MSG." The other day in Chinatown was a different story entirely. "Everyone uses some MSG," the waiter explains, just as cheery. "Every restaurant. Chinese, everyone else. If they say they're not," he pauses, "it's bull---t."
So, is the apparent and ongoing alarm well-founded? With the swirl of contending thought, it's difficult to tell. One thing's certain: MSG, the sodium salt of the protein glutamate, is, naturally, high in sodium. Not as high as salt (as the MSG side of the tracks points out). But it takes no conspiracist to tell you that a high-sodium diet increases the risks of all sorts of heart problems and hyper-tension, however it's consumed. People on a low sodium diet should "Read food labels. Buy products low in sodium, MSG . . ." urges, for instance, McKinley Health Centre at the University of Illinois.
For Keith Mitchell at Calico Foods, the sodium content in MSG and its ilk looked like an opportunity. "It's had a lot of bad press over the years, and people don't want it on their labels," he says.
That's why the company he works for is selling a low-sodium, amino acid-based flavour enhancer as an alternative. The problem: Sticker shock. "When you go to lower sodium, the flavour perception drops dramatically," he says. "It's one of the hardest things to replace – especially when it's practically free."
Indeed, salt – "one of the cheapest things going," Mitchell says – is a tough competitor to fight with pricey, innovative, low-sodium alternatives. "The business is not by any stretch of the imagination where I'd like to see it," he says. "For a company to reformulate everything and take salt out of its products takes time, and money. The industry is well aware of the issue. The question is, is the public willing to pay for it?"
Especially when, for all the consumer can see, MSG is perfectly safe. Nearly every regulatory agency, including the FDA in the U.S., has few issues with MSG. In 2005, the World Health Organization acknowledged that "neurotoxic effects have been seen in animal studies, but only at very high doses," often administered by injection; it concluded that "there is a substantial body of work investigating MSG at lower doses with no indication of any adverse effects."
Health Canada allows that "some individuals who consume MSG may exhibit an allergic-type reaction or hypersensitivity," but "(t)he safety of MSG has been studied worldwide.
"The Joint Food and Agriculture Organization of the United Nations / World Health Organization expert Committee on Food Additives (1987) and Federation of American Societies for Experimental Biology (1995) conducted thorough evaluations and concluded that use of MSG does not constitute a health hazard to consumers. Health Canada scientists concur with these views. In addition," it goes on, "contrary to some allegations found on certain websites, there is no scientific evidence linking obesity in humans with the consumption of foods containing this flavour enhancer."
That's what they want you to think, says Jack Samuels. Depending on whom you believe, Samuels and his wife, Adrienne, are either tireless champions of food safety, or obsessive conspiracy theorists with too much time on their hands (their self-directed anti-MSG lobby, "Truth in Labeling," has been described as both across the painfully vast swath of MSG opinion found in cyberspace).
Since 1971, when, Samuels says, he starting collapsing in certain restaurants after a meal – he concluded he was hypersensitive to MSG – the pair have campaigned endlessly against the additive. Samuels allows that he's a "very, very rare" type, to have these kinds of extreme reactions. "Most people would go through life and not have any kind of problem at all," he says. But, he says, speaking as someone "who can die" from eating MSG, he's pretty devoted to the cause.
Whether you choose to believe Truth in Labeling campaign information or not, Samuels makes a salient point. MSG is, at its base, a naturally occurring substance in all sorts of foods – tomatoes, Parmesan cheese, mushrooms, and, way back in 1908, kombu.
That was the seaweed Ikeda correctly suspected to be the source of a mysterious "fifth taste" in his soup, complementary but different from the basics – hot, sour, salty, sweet.
Distilling it to its base elements, he called the results umami – or "deliciousness" in Japanese. More than 35 years of research have told the Samuels that naturally occurring MSG – that is, the stuff Ikeda found – produces no reaction even in MSG-sensitive people.
When it's processed, as it most typically is, using fermentation or other chemical reactions, it frees the glutamatic acid from its protein compound, provoking some of the reactions its detractors claim.
For Frederick Oh, director of the Richmond Hill Culinary Arts Centre, therein lies the problem. "Over the years, the demand exceeded the supply and they started to make it chemically," he says. "That's where the problems started."
Whether they're as dire as the worst detractors suggest is nearly impossible to divine. Free glutamic acid – processed and unlinked from its base protein – is, like any chemically-created compound, hard for the body to absorb.
But for Oh, MSG's constant presence is more a symptom of a convenience-driven society that has neither the time nor the inclination to create authentic flavour.
"Making real stock – boiling down bones, doing it the right way – takes time, and it takes labour. Why bother if you can buy an enhancer for 10 bucks and you're done?" he says.
Oh says the issue is more than one of convenience. "We've developed a taste for it," he says. "Fat, salt, sugar – these are all the things we like to eat. MSG mimics those flavours. Nobody wants to eat plain-Jane food. If you open a restaurant advertising blandness, how long do you think you'll last?"
Ever-mindful of the MSG stigma the glutamate industry – a powerful lobby worth billions – has found a way to repackage itself, drawn from Ikeda's original soup test of a century ago.
Umami, they call it – a flavour increasingly finding its way into culinary lexicons and onto the pages of such magazines and newspapers as Gourmet and The Wall Street Journal, which said in an article in December that "(umami) was changing the way everyone from top chefs to Frito-Lay executives thinks about food."
So everything old is new again. "Give it a sexy name, re-package it and re-market it and you're on your way," Oh says. He sees us caught in a familiar catch-22.
"Everyone talks about the environment, but look at all the SUVs that are being produced," he says. "The whole world is in a predicament right now. We've become accustomed to living a certain way, at a certain cost. Will anyone have the guts to put on the brakes?"
************************************************
Where cancer-causing
agents lurk

What do cosmetics have in common with cellphones? They both worry a leading cancer scientist about their potential as health risks
Nancy J. White
Living Reporter
The Star
First off, Devra Davis won't do the interview on her cellphone.
Call me back on the land line, she instructs. It's not the money she's concerned about. It's the microwaves.
She's also concerned about drinking diet pop, wearing a lot of cosmetics and eating non-organic red meat.
But make no mistake: she's not some trendy health-scare type. She's a blue-chip cancer epidemiologist, director of the Center for Environmental Oncology at the University of Pittsburgh Cancer Institute with a Grade A scientific pedigree: a PhD from the University of Chicago, a decade at the National Academy of Sciences, an author of more than 170 published articles.
And she's worried about her environmental exposure to cancer.
"Everyone has to start where they're comfortable, taking control of their own homes," says Davis, who will be the keynote speaker at Women's College Hospital's health forum Friday. "Then they have to make sure they vote for politicians who understand the importance of this issue."
This issue is how we've let modern life, from the air we breathe to the products we use, poison our bodies.
"We've made remarkable progress in treating some forms of cancer," says Davis, 61. "But if we only improve our ability to find and treat the disease, without dealing with the underlying causes, we will not have made enough progress."
In her newest book, The Secret History of the War on Cancer, Davis argues that the long march against cancer has been misled too often by corporate interests and sidetracked by missed opportunities.
In 1936, more than 200 of the world's top cancer scientists convened in Brussels, a gathering of the best minds to create a new way forward in understanding and fighting the disease. When Davis unearthed the transcripts of those meetings, she was stunned to read how much those scientists knew about cancer's social and environmental causes.
Many widely used agents of the time, including ionizing and solar radiation, arsenic, benzene, asbestos, synthetic dyes and hormones, were recognized as cancerous in humans, she writes.
This knowledge came from researchers combining autopsies with medical, personal and workplace histories of cancer victims and conducting animal lab studies.
However, she says, these findings didn't seep into the mainstream medical practice of the day, due, in part, to the scant media coverage given scientific meetings back then. But mainly it was the timing, the brink of World War II. "The world had very different priorities," says Davis.
"Cancer is the ultimate long-term disease. To be concerned about cancer implies a certain optimism in the future."
In 1971, U.S. President Richard Nixon declared war on cancer, reflecting the idea that the type of ingenuity that built the A-bomb and put a man on the moon could wipe out cancer within the decade.
Rocket engineers from NASA held meetings with medical researchers, setting up charts with overlapping diagrams and lots of arrows, mapping out how the war on cancer should be conducted, writes Davis. Most serious researchers viewed the idea of a single cure as preposterous, a political fuss, she says.
The war did not take aim at any of the known or suspected carcinogens. Not even tobacco smoking, which the U.S. surgeon general had declared a cause of cancer in 1964.
"There were very close ties between the tobacco industry and, later the chemical industry, and the development of the war on cancer," she says.
Today, the emphasis is not so much on declaring war against cancer as it is dealing with a chronic condition, says Davis. "We need to make changes in the infrastructures of our lives that will help reduce the risks."
She's most worried about air pollution, such as emissions from coal-fired plants and growing vehicle traffic, that's distributed across the population. "It's important for people to understand that the burning of fossil fuels that's warming the Earth is the same process increasing our health risks, including cancer in the long term."
There are several other issues that concern her, particularly because health officials aren't paying much attention to them:
Cellphones – New data from Sweden, she says, show that people using cellphones for 10 years or more have double the risk of brain cancer. She's worried about kids under 16 glued to their cellphones. "Would you let your child play Russian roulette?" she asks.
Aspartame – The artificial sweetener's negative effects in animal studies occurred in the last third of the creatures' lives, which corresponds to human beings in their 60s to 80s. Again, she is especially concerned about children consuming the product over many decades.
The doses that induced cancer in animals, she says, were not especially high: about two cans of diet pop, two yogurts and a couple of sticks of gum a day.
Diagnostic radiation – The medical community is becoming increasingly concerned about unnecessary Computed Tomography scans of children, she writes. A CT scan of a child's stomach can be equivalent to 600 chest X-rays and one of an infant's head may equal a few thousand.
While a CT scan may well be warranted in a medical emergency, she says, repeated follow-up scans may not be a wise idea.
Ritalin – Several papers have indicated that Ritalin, valuable for treating Attention Deficit Disorder, might pose a risk to the user's genetic makeup, says Davis. In one study, researchers tested the blood of a dozen children before and after they were put on the drug, she writes, and found chromosome damage after three months' use.
Davis cautions that the numbers tested were small, no direct link to Ritalin was found and genetic damage and repair happens all the time. But given the widespread use of the drug in children, she says, governments and the private sector need to further investigate.
Overall, Davis believes the growing awareness of global climate change is sparking more concern about environmental health.
"The connection is obvious," she says.
"We only have one planet."
|







 Cost: $35
Cost: $35